Background: Delirium affects 20-60% of the general hospitalized patients, and up to 85% of intensive care unit (ICU) patients. Its occurrence is associated with higher morbidity and mortality, long-term institutionalization, worse long-term cognitive outcomes, and increased hospital length of stay and costs. It is often missed due to lack of standardization in assessment and diagnostic methods, and lack of awareness among physicians and other health care providers. Management is challenging due to differing subspecialty provider preferences, and limitations in current literature. There had been no standardized approach for prevention or management of delirium for non-ICU patients at our institution.
Purpose: To create and implement an evidence-informed collaborative MD-RN protocol for the prevention and management of acute delirium for non-ICU patients.
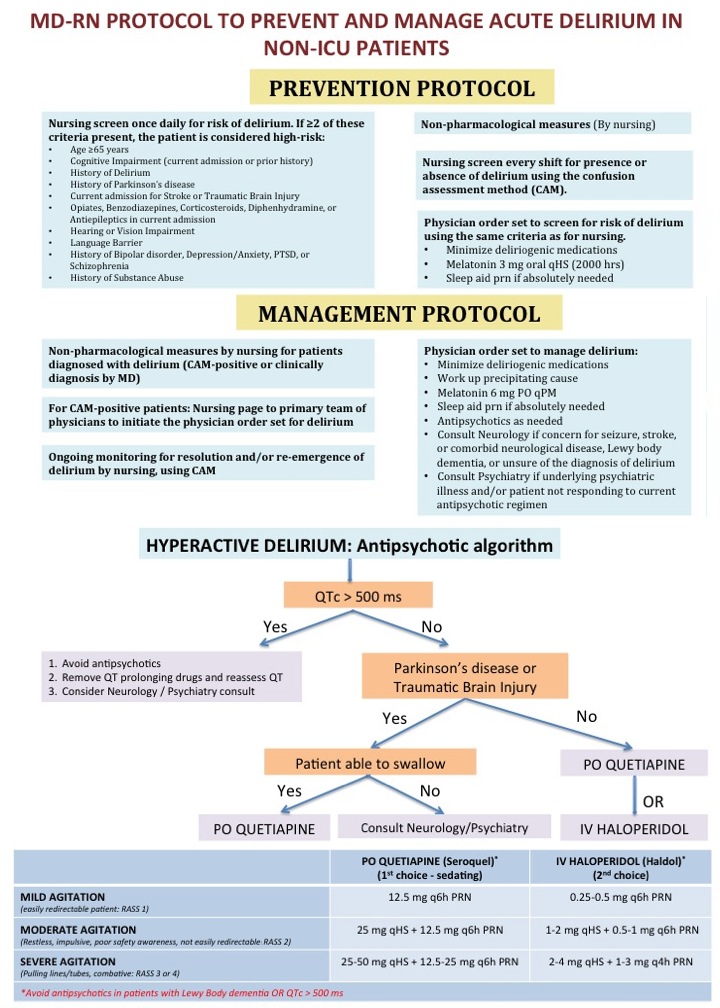
Description: In November 2013, we created a multidisciplinary delirium task force with representation from hospitalist service, psychiatry, neurology, neurosurgery, physiatry, pharmacy, nursing, quality/patient safety, and clinical informatics. Current institutional practice and literature were reviewed. Hospital-wide campaigns using didactic sessions to nurses and physicians have been held since to create delirium awareness. Educational materials have been posted on the intranet, and flyers and videos for patients and families have been created. Protocols for prevention and management of delirium in non-ICU patients were implemented on our electronic medical record system in June 2015. The prevention protocol comprises of: (a) Once daily nursing screening of all inpatients for risk of delirium, (b) Nurse-initiated non-pharmacological measures for delirium prevention in high-risk patients, including early mobility, reorientation, assuring sleep, noise reduction, bowel/bladder management, pain control, and caregiver education, (c) Nurse-initiated screening of all inpatients every shift for presence or absence of delirium using the confusion assessment method (CAM), and (d) MD order set for risk screening, ordering non-pharmacological measures by nursing, melatonin, and sleep aids if needed. If a patient was diagnosed with delirium, the management protocol is initiated: (a) Nurse-initiated non-pharmacological measures (same as in prevention protocol), (b) Nursing page to primary team of physicians to initiate the MD order set for delirium, (c) MD order set to work up the precipitating cause of delirium, order melatonin and/or antipsychotics as needed, and, (d) Ongoing monitoring for resolution and/or re-emergence of delirium by nursing using CAM.
Conclusions: A systematic and collaborative approach is essential to prevent and manage delirium. With this initiative, we created and implemented a MD-RN protocol feasible for use among hospitalized non-ICU patients. Further studies will measure the impact of this protocol on patient outcomes.