Background: There exists no standardized means of assessing hospitalist performance on quality, safety, efficiency and value metrics.Timely, accurate and meaningful feedback on individual performance is imperative to drive improvement.
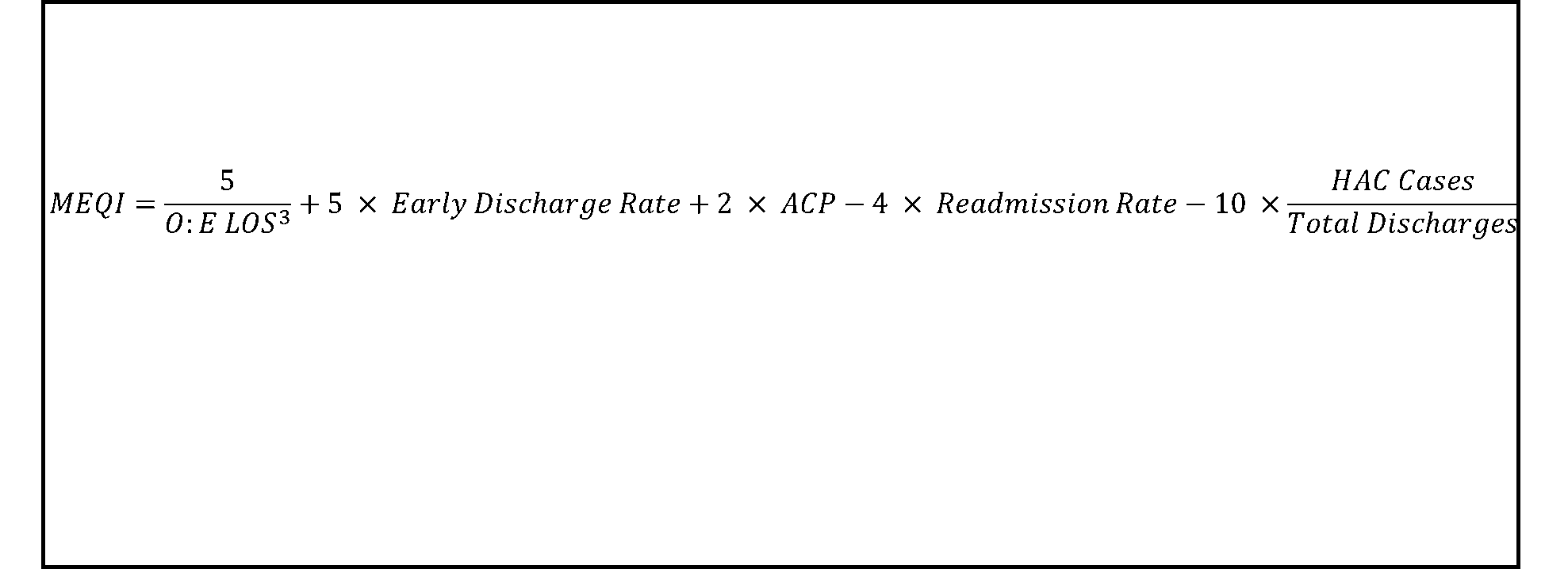
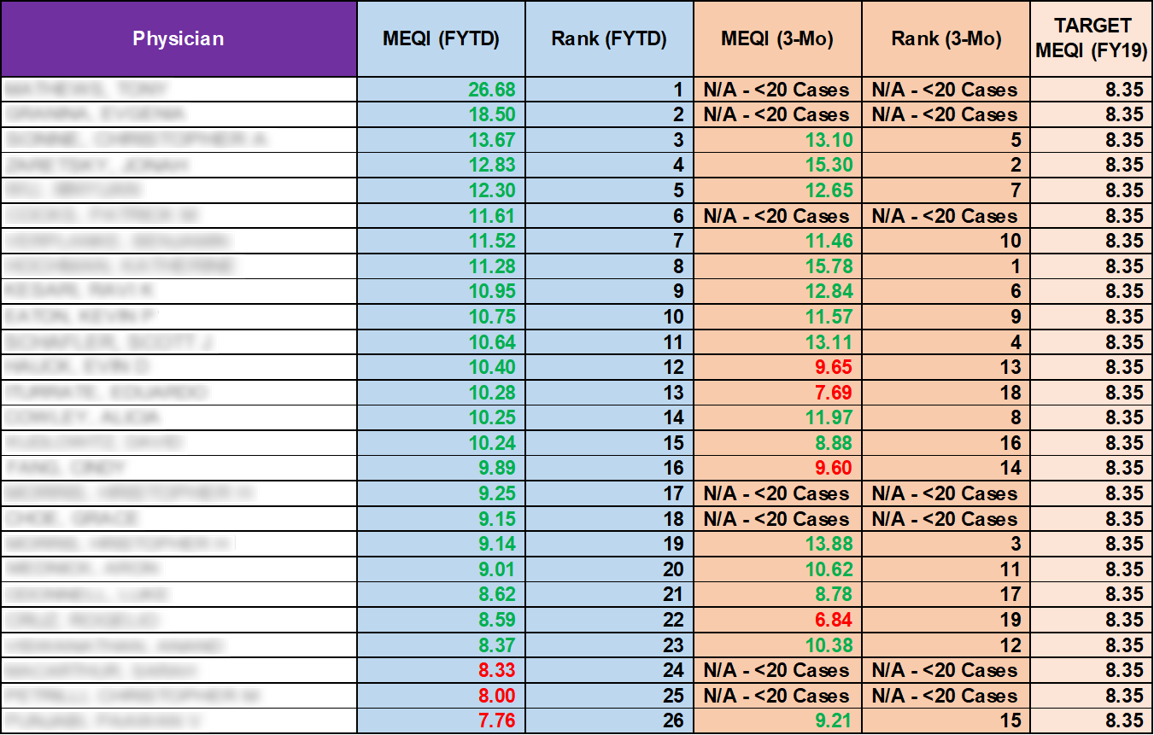
Methods: The components of the MEQI align with the institution’s most important metrics, including readmission rate, hospital acquired conditions and observed to expected length of stay. MEQI formula was developed in an iterative manner, weighted to reflect senior leadership with input from Hospitalist group. (Figure 1)The “Target MEQI” was calculated using institutional goals. Individual MEQI scores with full names were displayed at Hospitalist Faculty meetings on a quarterly basis. (Figure 2). Leadership developed careful messaging and a safe culture when delivering feedback. Mentorship was provided to “low performers” to aid in improvement.
Results: MEQI scores for hospitalist group increased from 9.58 (FY18) to 10.21 (FY19). Post-MEQI roll-out, the Variable Direct Cost per Case adjusted for CMI has decreased by hospitalist. Hospitalists are eager to receive feedback on their individual MEQI scores and improve.
Conclusions: Create a meaningful MEQI with (NOT for) your team. Let them become stakeholders. Transparency drives improvement. This can’t be negotiableLow performers respond to personalized feedback about their practice. MEQI 2.0 includes teaching evaluations; 360 evaluations from RN, Social Workers, Care ManagersMEQI for Inpatient Units under development and include HCAHPs, Empty bed Time