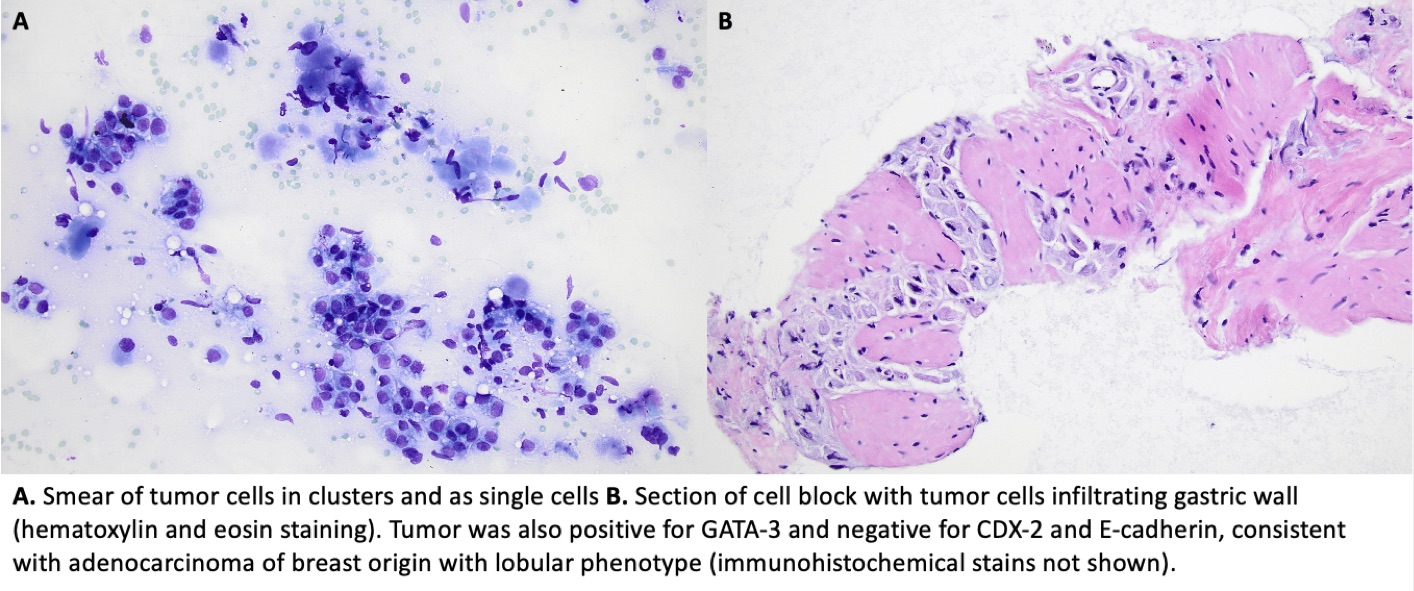
Case Presentation: A 56-year-old female with invasive lobular carcinoma of the breast, diagnosed 8 years prior and currently on neratinib and capecitabine, presented to her oncologist endorsing abdominal pain, vomiting, nausea, and loss of appetite for several days. Despite anti-emetic therapy, symptoms persisted, and she lost weight over the next 6 weeks. Computed Tomography (CT) showed gastric antrum thickening and intra/extrahepatic biliary ductal dilation. Magnetic Resonance Cholangiopancreatography revealed biliary wall thickening with tapering in the ampulla as well as areas of peritoneal lining thickening and omental edema. Esophagogastroduodenoscopy demonstrated an intramural/subepithelial lesion in the gastric antrum and prepyloric region with associated severe stenosis of the gastric antrum. Gastrojejunostomy and pyloric stent placement were performed. Fine Needle Aspiration (FNA) of the gastric lesion confirmed metastatic lobular breast cancer (Figure). She returned to the hospital 4 days after discharge with sharp epigastric pain. Labs showed new elevations in lipase >3000 U/L, alkaline phosphatase 350 U/L, total bilirubin 1.9 mg/dL, and AST/ALT 569/362 U/L. CT showed interval increase in gallbladder distention. Endoscopic Ultrasound and Endoscopic Retrograde Cholangiopancreatography showed severe duodenal stenosis and main bile duct and pancreatic duct strictures, which were dilated and stented. It was postulated the duodenal stenosis was due to submucosal cancer infiltration, as was the case for the gastric lesion, although biopsy was not performed at this time. Procedural recovery was complicated by diet intolerance, which prompted a repeat CT that showed dilation of the jejunum with areas of narrowing concerning for malignant partial small bowel obstruction. Total parenteral nutrition was initiated. Over the next month, chemotherapy was resumed and the patient gradually tolerated a diet again. Biopsies of omental and peritoneal lesions were later obtained; results also confirmed metastatic lobular breast cancer.
Discussion: While breast cancer is the most common malignancy diagnosed in women worldwide, metastasis to the gastrointestinal (GI) tract is rare. Moreover, diagnosis is challenging because symptoms are often nonspecific, and GI metastasis from primary breast cancer may clinically and radiologically mimic primary GI tumors [1-4]. Establishing the correct diagnosis is essential for selecting appropriate treatment; primary gastric cancers are typically treated with surgical intervention while breast cancer metastases are treated with systemic chemotherapy [1,3].Knowing when to suspect GI metastasis from primary breast cancer is critical. Studies have shown that gastric metastasis occurs more often with lobular, compared to ductal, breast cancer [4-5]. The reported average time from breast cancer diagnosis to GI involvement varies across literature, ranging from a median of 41 months to approximately 6-7 years [3,6-7]. This case is an incidence of GI metastasis presenting 8 years after diagnosis.
Conclusions: We present a case of diffuse GI metastases causing abdominal pain, nausea, and anorexia in a patient diagnosed with invasive lobular carcinoma of the breast. While rare, GI metastasis should be on the differential for breast cancer patients with nonspecific GI symptoms refractory to supportive treatment, particularly if the cancer is lobular phenotype.