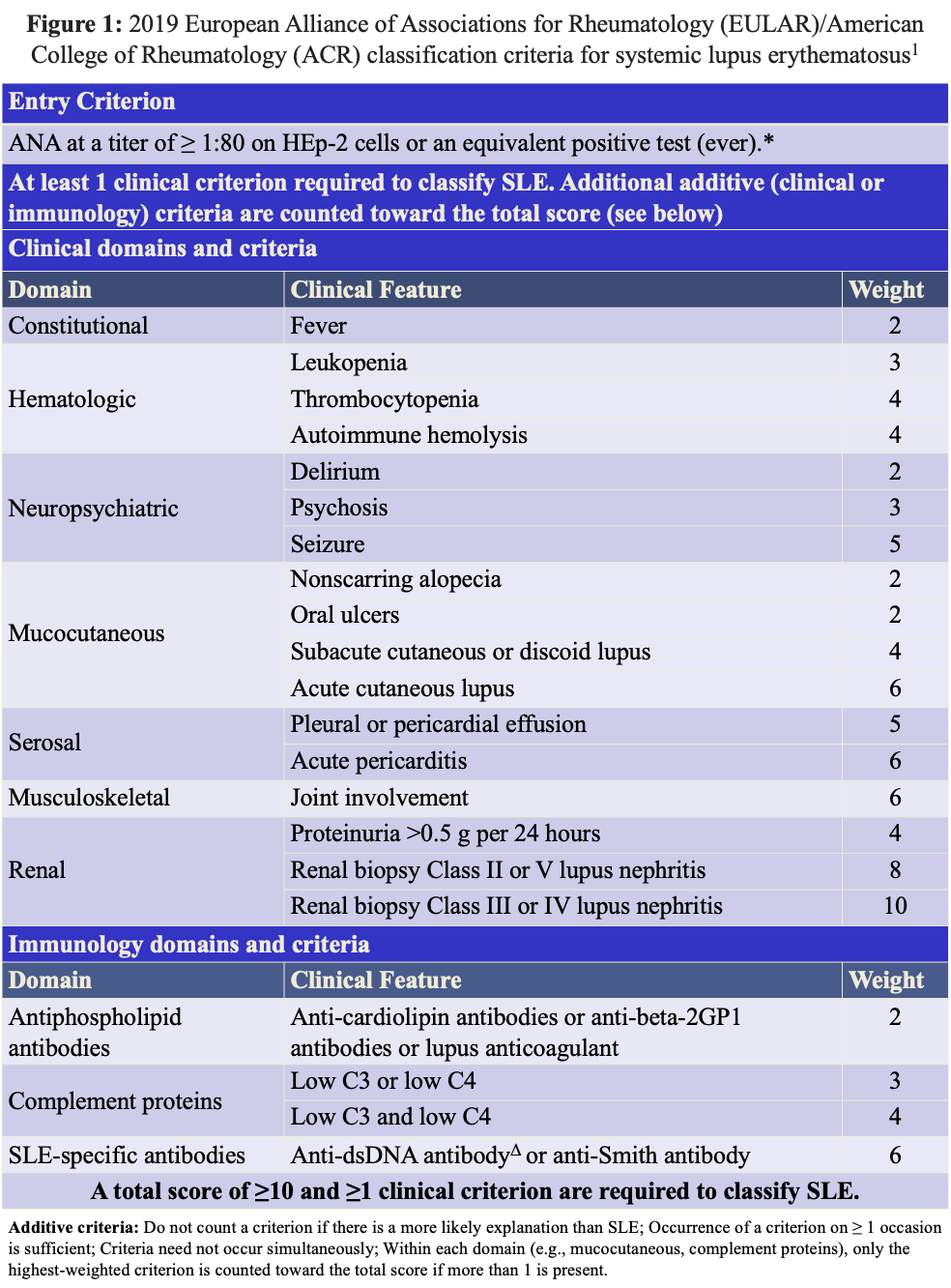
Case Presentation: Systemic lupus erythematosus (SLE), commonly known as lupus, is a multifaceted autoimmune disorder characterized by a myriad of clinical manifestations, including but not limited to fatigue, joint pain and swelling, and malar rash. Although a common cardiac manifestation of SLE is pericarditis, often accompanied by pericardial effusion, pulmonary arterial hypertension (PAH) is not often the original presenting manifestation of SLE.A 28-year-old female with no significant past medical history was admitted to the hospital due to new onset dyspnea on exertion and tachycardia with concern for pulmonary hypertension and large pericardial effusion. Review of systems was notable for fevers, a dry cough and an intermittent hot, tingling sensation in her fingers. On physical examination, she was tachycardic with wavering oxygen saturations (94%-100% on room air). Her exam was otherwise unremarkable. Her initial labs were notable for anemia (Hgb 10.5), thrombocytopenia (Plt 68k), elevated BNP (1061), and elevated LDH (297). Bedside transthoracic echocardiogram showed a large pericardial effusion with elevated right sided filling pressures and right ventricular hypertrophy. Given the patient’s acute presentation, the cardiology team performed a right heart catheterization, which confirmed PAH (mean PA pressure 44, PVR 4.2 Woods units). Her rheumatologic workup revealed a positive ANA screen with homogenous ANA pattern (1:2560), positive anti-dsDNA Ab (1:640), positive Smith Ab, positive Smith/RNP Ab, positive SSA/Ro, and positive rheumatoid factor. Additionally, she had low complement levels, C3 and C4, at 62 and 8.0 respectively. She met ACR/EULAR 2019 criteria for SLE with 21 pts (see Figure 1). She was treated with a prednisone taper and hydroxychloroquine. Additionally, she was given sildenafil and furosemide for the treatment of her PAH. The patient showed improvement after initiation of treatment and was discharged with close follow up with rheumatology and pulmonology follow up.
Discussion: Our otherwise healthy patient presented pulmonary arterial hypertension and large pericardial effusion. Multiple causes of pulmonary hypertension were considered, including left heart disease (Group II), pulmonary embolism (Group IV), chronic lung disease (Group III), and autoimmune etiology (Group I). Given her lack of medical comorbidities and positive rheumatologic workup, her symptoms were attributed to her newly diagnosed SLE.
Conclusions: Although rare, SLE should be considered in patients presenting with pulmonary hypertension and pericardial effusion who are lacking other risk factors. Early recognition and treatment of this rare cardiovascular manifestation could lead to a lower mortality and better prognosis.