Background: Communication between Hospital Medicine physician teams and interdisciplinary care providers (e.g. nurses, physical and occupational therapists, case managers) regarding disposition planning is often inconsistent, potentially delaying care and resulting in poor patient and provider experience. Prior studies demonstrate that sharing the estimated discharge date (EDD) early in a patient’s hospitalization can improve communication and interdisciplinary planning for discharge. Electronic medical record (EMR)-based tools are available to facilitate discharge planning but are variably used by Hospital Medicine teams at our institution. We aimed to improve effective utilization of EMR-based tools to communicate disposition plans between resident teaching teams and the interdisciplinary team.
Methods: An EMR-based EDD tool (Epic, Inc) was developed at our institution, an urban academic teaching hospital with up to 16 patients each across 8 teaching teams in Hospital Medicine, and was accessible by physicians, case managers, and nurses. Based on literature review, the study team set the intervention goal to increase the EDD accuracy within 24 hours of discharge for patients on the Hospital Medicine teaching service, from a baseline of 45% to a target of 63% of patients for at least two-thirds of the duration of intervention. Using LEAN methodology, or principles to optimize workplace efficiency, the study team completed a gap analysis and outlined key countermeasures. Core interventions targeting resident physicians and case managers were developed based on pre-intervention surveying with stakeholders including education (flyers, emails, orientation slides), gamification, and automated weekend reminders to update EDD. EDD accuracy was measured biweekly through EMR-based data extraction. Residents were surveyed pre- and post-interventions, and semi-structured interviews and surveys were completed with case managers post-intervention.
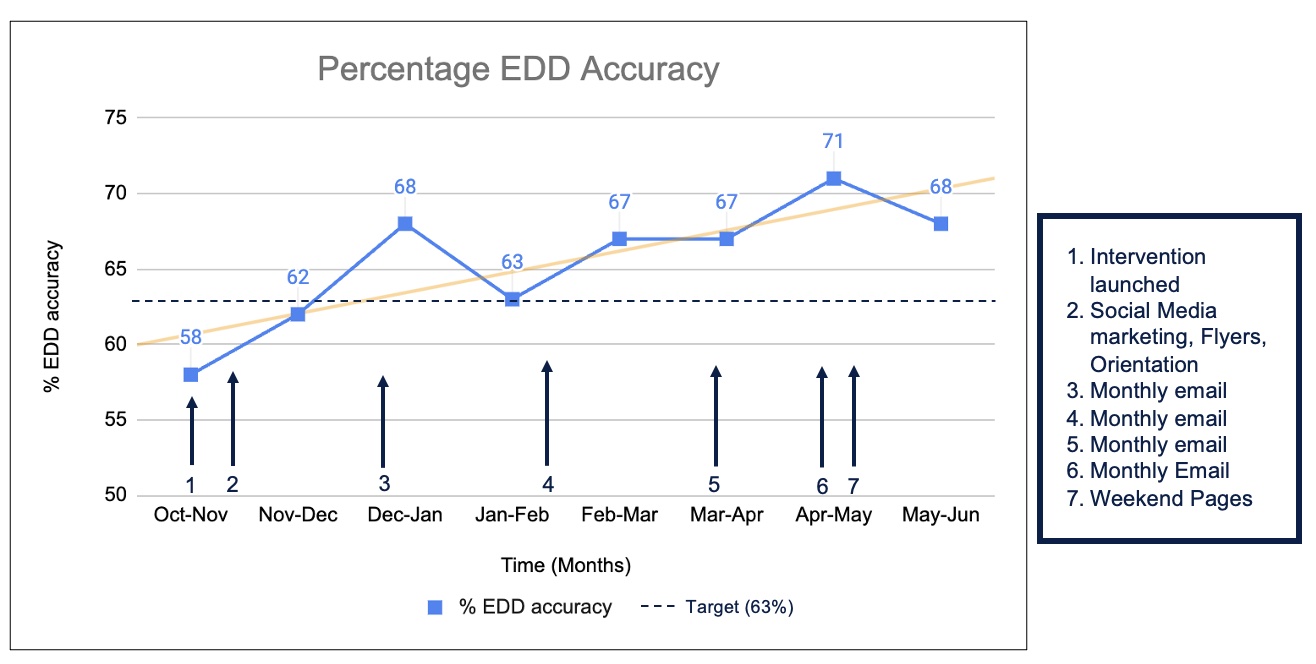
Results: In the pre-intervention phase (n=21), 38% of residents were familiar with EDD, 0% were aware of how to update the EDD, and 19% had interacted with the EDD feature on the EMR. In the post-intervention phase (n=20), 83% of residents updated the EDD at least 1-2 days of the week and 88% of residents verbally communicated the EDD during daily interdisciplinary rounds. Surveys with case managers demonstrated that 88% of case managers updated EDD on most or all weekdays, but only 25% updated EDD on weekends. Semi-structured interviews highlighted that updating the EDD led to a more explicit shared goal for patient disposition. Overall, EDD accuracy across resident teams improved by 17% over the 8 intervention months (Figure 1), with EDD accuracy above the target of 63% for over half the duration of the intervention.
Conclusions: EDD accuracy across resident teams improved with promoting the use of an interdisciplinary communication tool embedded in the EMR, enabling a shared understanding of a targeted discharge date and creating a cultural shift in communication with the aid of the EMR. Our study demonstrated that EMR-based tools that specify EDD can promote interdisciplinary provider communication and collaboration around discharge planning and increase visibility of EDD for all care team members. With a shared, accurate EDD goal, inpatient teams can avoid common discharge pitfalls and cohesively communicate with patients around next steps in care.