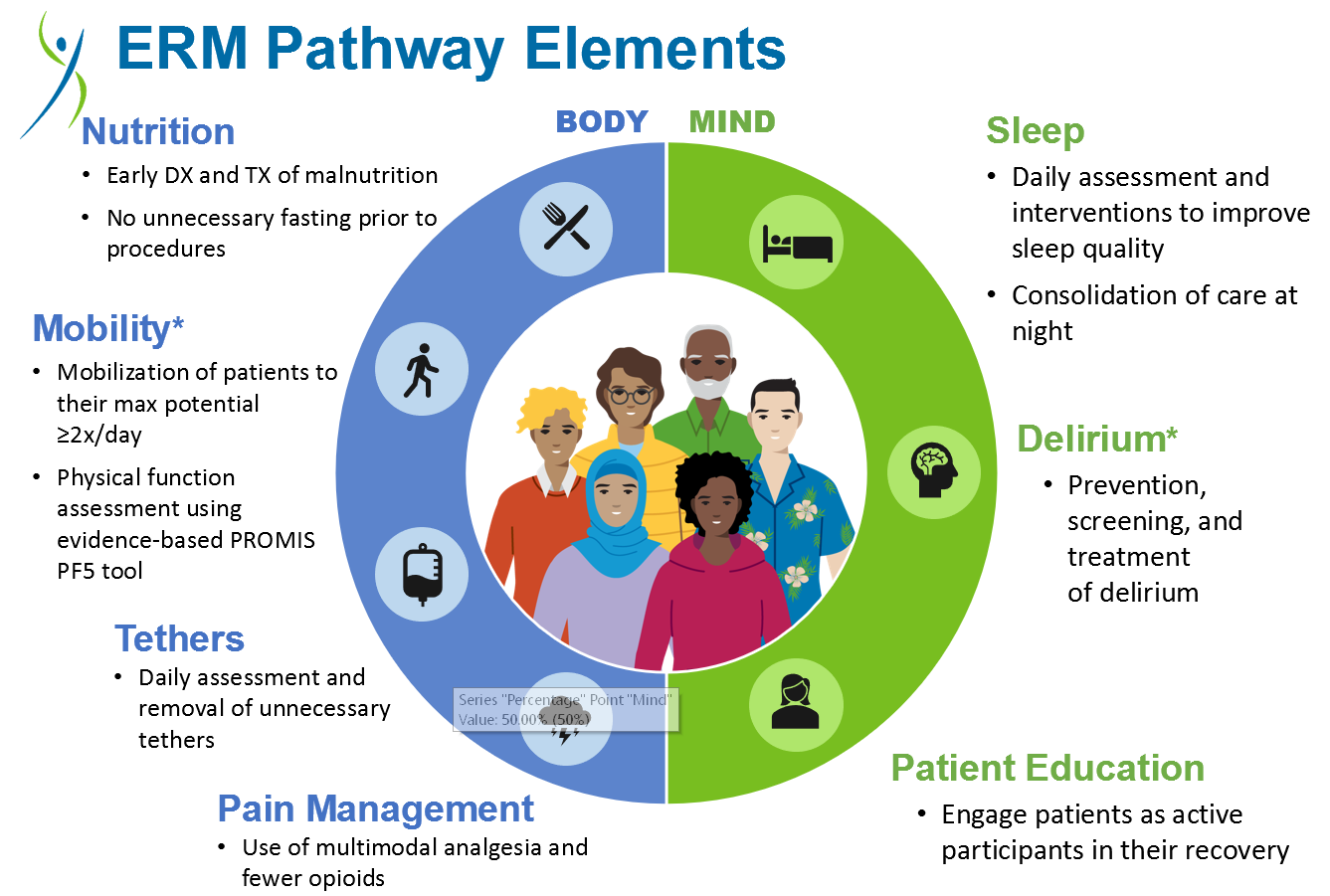
Background: In May 2022, Kaiser Permanente introduced “Enhanced Recovery Medical” (ERM). Modeled after “Enhanced Recovery After Surgery,” (ERAS), ERM aims to reduce hospital-acquired debility. Predefined ordersets and modified workflows help healthcare teams optimize elements key to recovery: nutrition, mobility, tethers, pain, sleep, and delirium. This ongoing quality improvement (QI) project examines how a resident-led initiative impacted co-resident awareness, attitudes, and behaviors towards ERM.
Methods: Using Institute of Healthcare Improvement (IHI) methodology, the project consisted of PDSAs and measures aligned with those tracked institutionally by the ERM program. The patient population included adults on medical-surgical floors. The project began with an educational curriculum for the program’s residents, where sessions discussed each ERM element (i.e., “mobility”) and collected feedback. Resident input led to the first iteration of a novel refreshable “Bundle” smartphrase which pulled ERM elements into documentation. Some parts of the Bundle had forcing functions to free text specific orders (e.g., bowel regimen). Others automatically pulled data into the note (e.g., presence of a tether such as telemetry). Surveys captured resident feedback from both the 2022-23 (April/May) and 2023-24 academic years (September/November). Preliminary data describe changes in awareness of ERM elements after the educational campaign as well as before and after the creation of the Bundle smartphrase.
Results: During the education PDSA, survey results showed tether awareness improved 29% in spring 2023 with a statistically significant increase (65% to 94%, p=0.05) in fall 2023. Awareness of multimodal analgesia (MMA) for pain management improved in spring (48% to 76%) and in fall 2023 (35% to 67%); however, the observed change was not statistically significant (p=0.06). Residents’ familiarity with patient mobility, ranging from ‘somewhat’ to ‘very’ familiar, increased 15% in spring 2023 and 7% in fall 2023 (not statistically significant). Despite overall low levels of smartphrase utilization, uptake gradually increased (12% in May, 35% in September, and 39% in November). Hospital-wide, tethers rate decreased from an average of 1.6 in January 2023 to 1.5 in October 2023. In the same period, percentage of patient encounters using MMA increased from 36.0 to 43.7. Average mobility increased from 3.6 to 4.0. Finally, the percentage of encounters with delirium diagnoses after hospitalization, a balancing measure, decreased from 16.3 to 14.1.
Conclusions: Results suggest that the educational campaign may have enhanced awareness; however, resident practices alone did not improve hospital trends as nursing and ancillary staff contribute significantly to ERM. Data interpretation is also limited because surveys attained different numbers of respondents. While most residents did not incorporate the smartphrase, the changes in awareness demonstrate that the residency program prioritizes minimizing hospital-acquired debility. Future work will target potential obstacles to sustaining this cultural change.