Background: Financial incentives motivate hospitals to focus on improving patient experience, quality indicators, and efficiency metrics. Efforts to geographically staff hospitalists have renewed the focus on quality improvement efforts at the inpatient unit level. However, in order to maximize the benefit of geographic staffing, a unit-level leadership structure and quality-improvement support system must be developed. Physician consistency creates an opportunity to cultivate a leadership dyad between the physician and the nurse manager on the unit. Equipping the physician-nurse co-leads with systems engineering support provides the necessary foundation to develop an Accountable Care Unit; a unit that independently and continually works on process improvement.
Purpose: To reduce the length of stay by structuring an inpatient unit as an Accountable Care Unit, a unit with physician-nursing co-leadership and systems engineering support that allows for sustained process improvement.
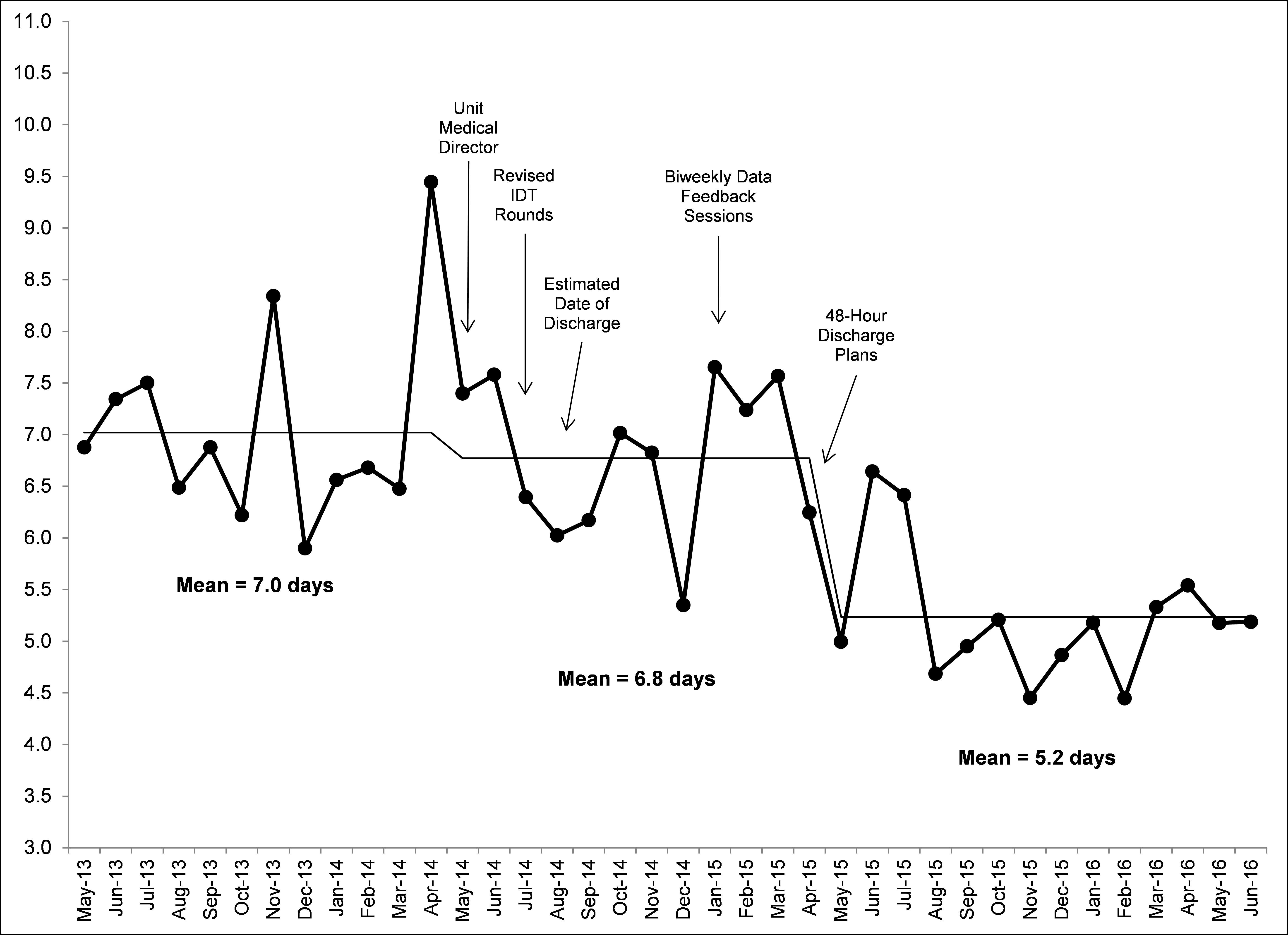
Description: On a 39 bed medicine unit with an average daily census of 41 we developed an Accountable Care Unit model from 2014 to 2016. Prior to May 2014, a unit had monthly rotating hospitalists. Minor variations in the practice of providers led to process inconsistencies. In May 2014, with the help of geographic staffing we implemented a permanent physician on a unit known as the Unit Medical Director (UMD). The UMD is a geographically assigned attending physician who works on one unit and partners with the Administrative Nurse Manager (ANM) to achieve unit goals while maintaining full clinical responsibilities. With the support of a performance improvement specialist offering continuous data feedback, the UMD and ANM designed and implemented numerous process changes over the course of a year. These changes included structured interdisciplinary rounds, identifying an estimated date of discharge (EDD) for each patient each day, defining 48-hour discharge plans that specified team member responsibilities, and developing scheduled and structured communication tools. Length of stay (LOS) was monitored with each intervention. Successful interventions were adopted into the Accountable Care Unit structure. The LOS for the year prior to experimentation was 7.0 days. During the year of experimentation, LOS decreased to 6.8 days and following the permanent changes, LOS was 5.2 days.
Conclusions: The Accountable Care Unit model improved length of stay by 1.8 days. Geographic staffing and physician consistency established a physician-nurse leadership dyad. Partnered with systems engineering support, this co-leadership model led to sustained unit-level process improvement.