Background: Hyperglycemia in hospitalized patients is well-known to be associated with adverse outcomes, such as infectious complications, increased length of stay, and increased mortality. To that effect, aggressive treatment of inpatient hyperglycemia has been shown to improve outcomes in both Medicine units and MICU. This study aimed to identify the number of patients experiencing persistent hyperglycemia in inpatient units at the University of Missouri-Columbia hospital, implement an effective cross-disciplinary protocol to achieve better glycemic control, and monitor outcomes from these measures.
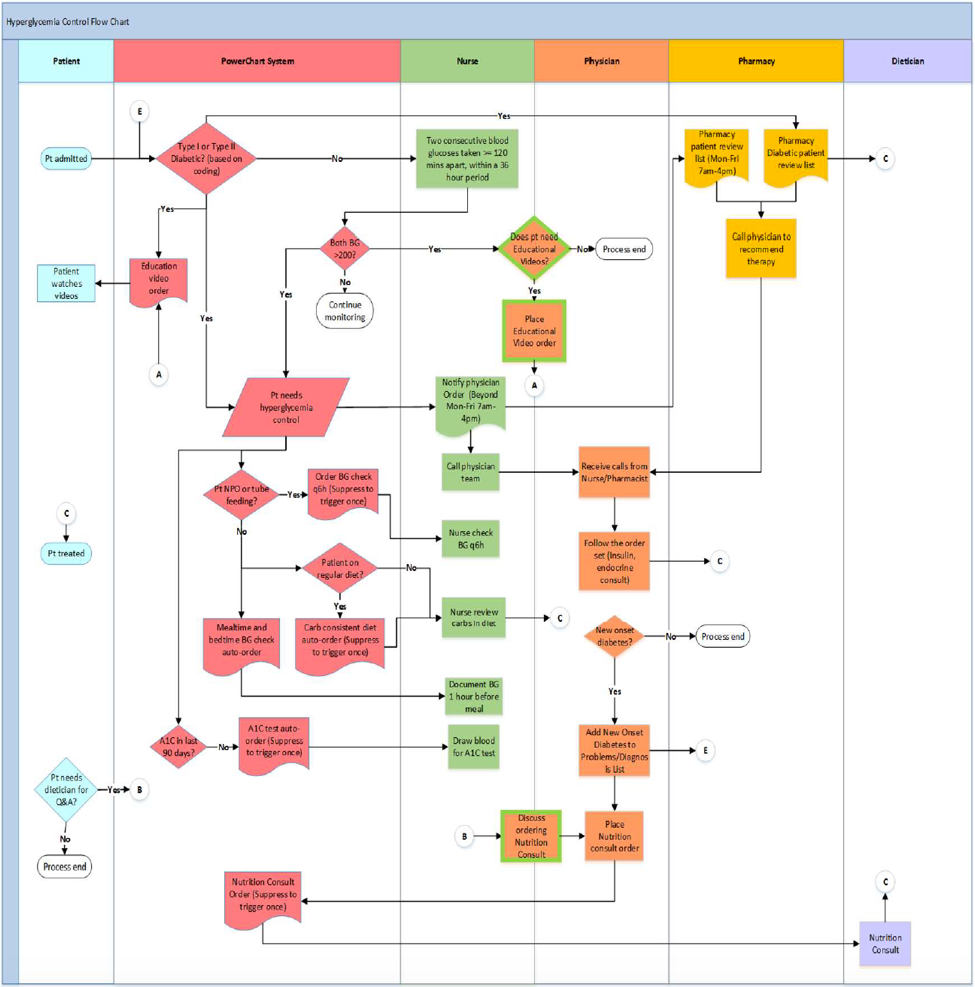
Methods: The control group consisted of Type-1 (T1DM) or Type-2 (T2DM) diabetics present on the Cardiology unit or Cardiology ICU between June 2017-January 2018. The intervention group consisted of patients on these same floors after August 2018 identified based on 1 of 2 criteria: diagnosis of T1DM/T2DM or having had at least 2 consecutive blood glucose (BG) readings >200 mg/dL within 2-36 hours apart. Patients fulfilling either criteria were excluded if diagnosed with DKA or HHNK, as well as if on IV insulin. Upon patient admission, the following were automatically placed via EMR: diabetes education (dietary, nursing, and videos); pharmacy medication review; basal, bolus, and correction scale per pharmacy recommendation; hemoglobin A1C level if undocumented within 90 days; and carb-consistent diet with mealtime and bedtime BG checks.
Results: In our control group, 475 and 212 T1DM/T2DM patients were present on the Cardiology and CICU floors, respectively, with 171 (36%) and 70 (33%) patients who experienced 2 consecutive BG readings >200 between 2-36 hours apart. In our intervention group from August-October 2018, 154 and 71 T1DM/T2DM patients were present, with 57 (37%) and 25 (35%) patients who experienced the hyperglycemia event. 22% and 13% of patients in these groups experienced >10 instances of this hyperglycemic event pre-implementation, while this occurred in 11% and 20% of patients post-implementation. Average length of stay (ALOS) decreased from 5.6 and 6.6 days pre-implementation to 5.3 and 5.2 days post-implementation. Post-implementation analysis after 3 months showed 75% of Cardiovascular staff and 68% of CICU staff read the developed protocols. In addition, this analysis showed that of the 40 patients who triggered a pharmacy medication review alert, only 27 (68%) patients were successfully reviewed by a pharmacist.
Conclusions: The design and implementation of this large-scale protocol change required 9 months of refinement and delegation among various disciplines. A pilot study in the Cardiology unit and Cardiology ICU was chosen before dissemination to other units. Post-intervention analysis has shown improvements in chronicity of hyperglycemic events in only the Cardiovascular unit and ALOS in both units. These results may be influenced by suboptimal protocol understanding by staff and pharmacy review of patients, overflow from other units that are not included in the intervention but are included in these units, and a small sample size. As we continue to monitor the progress of this pilot study, special attention will be paid to 30-day readmission rate, length of stay, rate of serious infection, mortality, and the aforementioned BG parameters.