Background: In November 2020, CMS issued the Acute Hospital Care in the Home waiver which allows hospitals to care for appropriate Medicare inpatients in a patient’s home. UNC Health launched its home hospital program Advanced Care at Home in August 2021. Hospitals issued the CMS waiver are required to subject patients to both clinical and social screening to evaluate their appropriateness for care under this model. Understanding the reasons patients are not felt eligible can reveal opportunities for improvement to expand the population that can be cared for in a home hospital program.
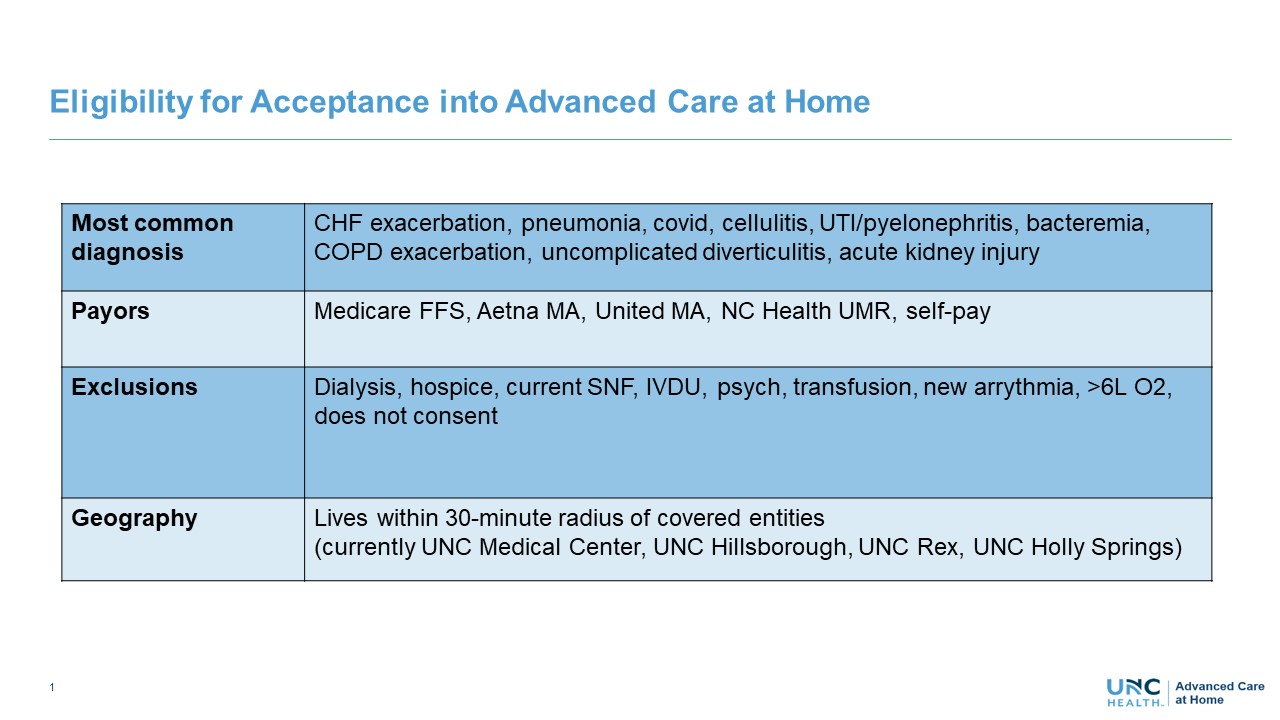
Methods: In April 2022, Advanced Care at Home added a question to its EMR screening tool to capture the reason a patient was screened out for the program (see Figure 1 for eligibility criteria). The screening tool was completed by a physician or nurse from the Advanced Care at Home clinical team and was completed through review of the EMR and sometimes with supplemental information from the hospital clinical team, from the patient or from a family member. Answer choices in the tool were based on common reasons for ineligibility seen in the prior months, including clinical reasons (ie. Need for dialysis), social reasons (ie. Skilled nursing facility resident), waiver requirements (ie. Observation status) and decline of the program by the patient or hospital clinical team. Patients undergoing this screening had already been determined to live in the geographic catchment area and to have an eligible payor. The results of this screening were tabulated over a five-month period (April – July 2022).
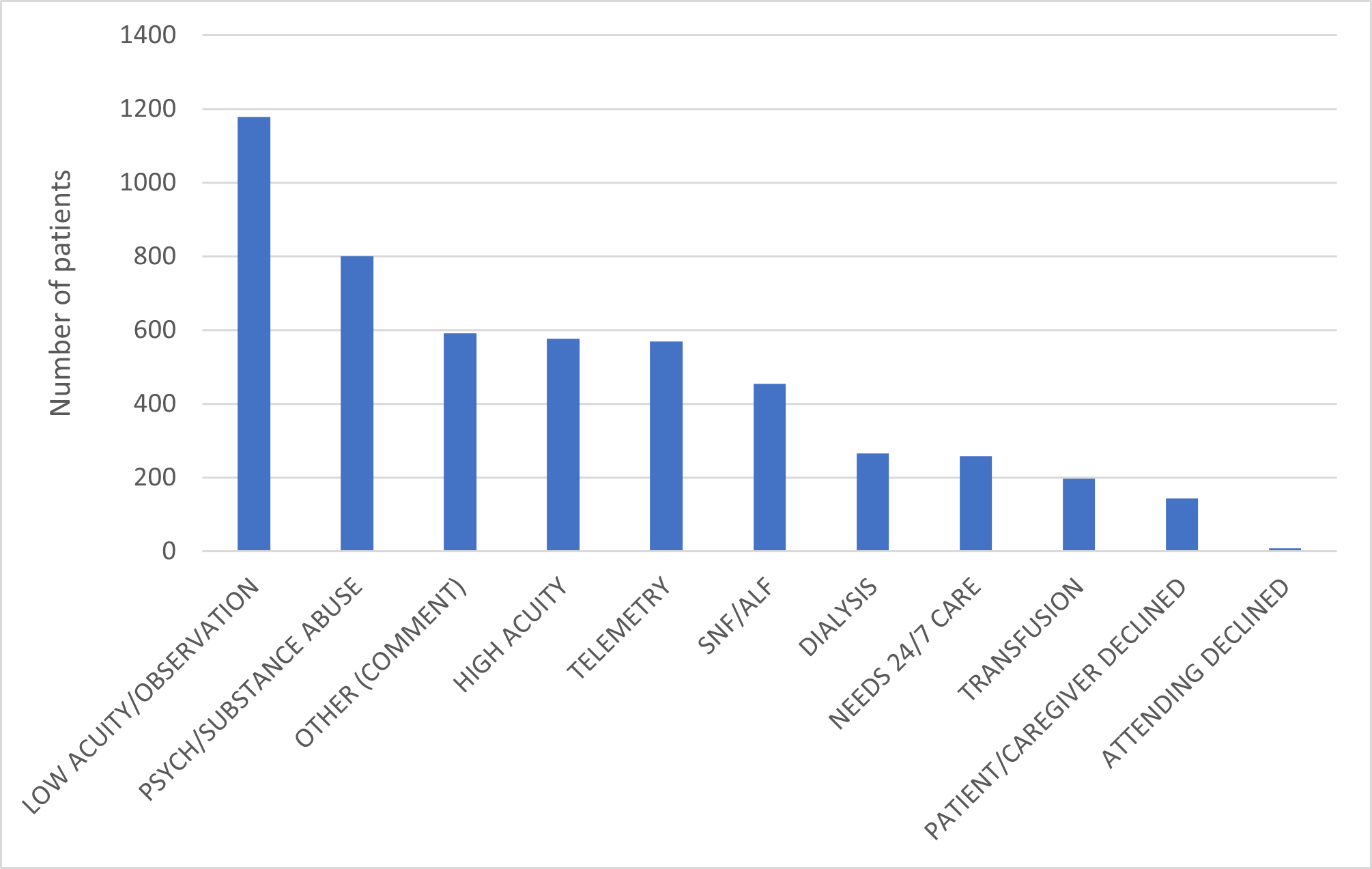
Results: During the data collection period, the questionnaire tool was completed on 5044 patients who were evaluated for Advanced Care at Home but ultimately screened out. The leading reason for being screened out was “Low acuity/observation” with a total of 1178 patients (23.4%). This was followed by “Psych/substance abuse” with 800 patients (15.7%), “Other” with 591 patients (11.7%) and “High acuity” with 577 patients (11.4%). The least common reason was “Attending declined” with 8 patients (0.2%). Figure 2
Conclusions: Our data collection showed patients were screened out from our home hospital program for a variety of reasons. While some of these barriers may be challenging to overcome, others are opportunities to expand this care model to a greater number of patients. This includes both through advocacy to CMS (to allow for observation level care or care in skilled nursing facilities) and through expansion of clinical services (ie. telemetry, dialysis, aides). Our results can help focus on the opportunities with the greatest possible impact.