Background: Hypoglycemia is common and potentially life-threatening for diabetic patients, often iatrogenic from diabetes treatments. It is important to be able to accurately study rates of hypoglycemia when evaluating the inpatient treatment of diabetes at a systems-level. Discharge diagnosis codes show promise as a tool in the surveillance of hypoglycemic events in large administrative databases and have been utilized in many studies for that purpose. The aim of this study is to validate inpatient diagnosis codes with laboratory-measured hypoglycemia.
Methods: The study population consisted of adults with diabetes admitted to a Veterans Health Administration hospital from 2016 to 2022. Information collected included demographics, discharge diagnosis codes, outpatient comorbidity diagnostic codes, laboratory glucose values, and mortality data. Hypoglycemia diagnosis was based on ICD-10-CM diagnostic codes for hypoglycemia. Laboratory hypoglycemia was defined as plasma glucose less than 70 mg/dL [3.89 mmol/L], consistent with guideline recommendations. Severe laboratory hypoglycemia was defined as plasma glucose less than 50 mg/dL [2.78 mmol/l]. Logistic regression was used to analyze odds of 30-day and 1-year mortality, controlling for demographics and comorbidities.
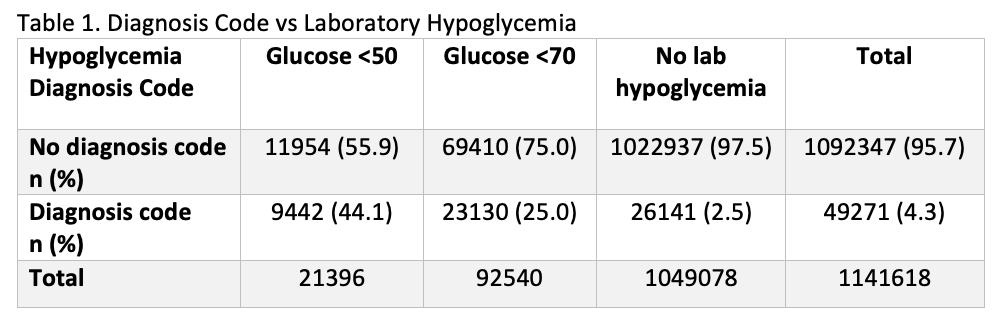
Results: 1,141,618 hospitalizations were identified, with 49,271 (4.3%) having a hypoglycemia inpatient diagnosis, 92,540 (8.1%) with laboratory hypoglycemia, and 21,396 (1.9%) with severe laboratory hypoglycemia. Hypoglycemia diagnosis codes were more commonly observed amongst Hispanic and Black patients, occurring in 4.7% and 5.4% respectively, compared to 3.9% in hospitalized white diabetic patients. Severe laboratory hypoglycemia was also more common amongst Hispanic and Black patients, 2.3% and 2.4% respectively, compared to 1.6% for white patients (p-value <.0001). Only 25.0% of those with laboratory hypoglycemia and 44.1% with severe laboratory hypoglycemia were found to have a hypoglycemia discharge diagnosis. Including laboratory and severe laboratory hypoglycemia increased identified hypoglycemic patients by 140.9% and 24.3% respectively. Laboratory hypoglycemia was associated with odds ratio 1.75 (95% CI 1.71-1.80) for 30-day mortality and 1.69 (95% CI 1.66-1.71) for 1-year mortality.
Conclusions: Based on this analysis of a large, nationwide healthcare system, discharge diagnosis code-based surveillance significantly underestimates inpatient hypoglycemic events, missing 75% of patients with hypoglycemia and 55.9% with severe hypoglycemia by laboratory measurement. Blood glucose < 70 mg/dL is typically treated with some intervention in the inpatient setting and could therefore be considered clinically significant. Additionally, laboratory hypoglycemia < 70 mg/dL was significantly associated with both short-term and long-term mortality in this study.Surveillance of inpatient hypoglycemia is important to monitor for potential harm from inpatient diabetes treatment, with significant implications for clinical decision-making and system-level patient safety measures. While routinely collected and less costly compared with resource-intensive adjudication efforts, discharge diagnosis codes will significantly under-estimate inpatient hypoglycemic events based on this analysis, and therefore additional measures such as laboratory surveillance should be employed as well for systems-level monitoring.