Background:
Death in the United States frequently occurs in institutions, despite the majority of persons indicating a preference to die at home. Little research has examined how well individual preferences compare with actual site of death. We sought to determine independent predictors for agreement between preferred and actual place of death among a population of hospitalized adults.
Methods:
This observational cohort study recruited patients admitted to the general medical service at the University of Colorado Hospital, Veterans' Affairs Hospital and Denver Health Medical Center (safety net hospital) in the Denver metropolitan area from 2003 to 2005. Patients who spoke English or Spanish, were able to consent, and were admitted for more than 24 hours were invited to participate in a brief interview that included a question about where they preferred to die. Follow‐up data on date and site of death were collected from 2005 to 2009 from hospital records and death certificates. Chi‐square tests were utilized to determine associations between concordance of preferred and actual site of death and patient level characteristics, including ethnicity, socioeconomic status, education, severity of illness, presence of an advance directive (AD), and hospital setting. Variables with a P < 0.25 were selected for logistic regression modeling of predictors of concordance.
Results:
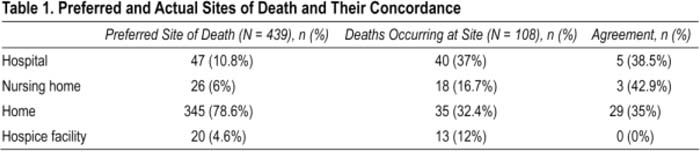
We enrolled 439 patients with a mean age of 58 ± 15 years; 35% (n = 159) were female, 19% (n = 88) were African Amencan, and 22% (n = 102) were Latino. One hundred and twenty‐three subjects died during the study period; complete death records were obtained for 108. The vast majority wanted to die at home as opposed to any other location. Although almost 79% expressed a preference for dying at home, only 32% of deaths occurred at home, and only 30% died in their preferred site (Table 1), In logistic regression modeling, the only significant predictor of concordance between preferred and actual site of death was the presence of an AD in the medical record [odds ratio 2.8 (95% Cl 1.1–7.2)].
Conclusions:
The majority of patients did not die at their site of preference. The presence of an AD in the medical record appeared to be the sole predictor of concordance between preferred and actual site of death. Understanding whether the AD directly influences site of death, as opposed to those persons likely to complete an advance directive simply being more inclined to effectively communicate their preference to care givers and family, is essential for advocating for more pervasive use of ADs, A prospective RCT to determine if ADs can increase site of death concordance is an essential next step in improving end‐of‐life care in the United States.
Author Disclosure:
L. Cervantes, none; J. Kutner, none; A. Sauaia, none; S. Fischer, none.