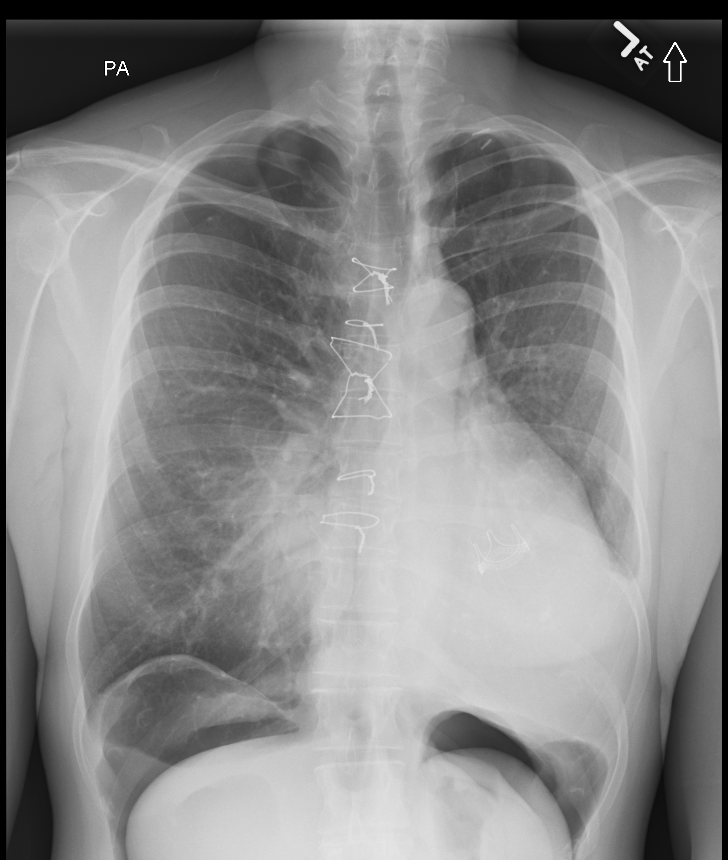
Case Presentation: A 36-year-old woman with Loeys Dietz Syndrome (LDS) presented with complaints of a “gurgling” sensation in her right chest. Her medical history included an aortic root aneurysm repair, aortic valve replacement and pneumothorax treated with chest tube. Physical exam demonstrated pectus excavatum and a rub throughout all right lung fields. Chest X-ray revealed a small right apical pneumothorax and large volume pneumoperitoneum. CT scan of the chest, abdomen, and pelvis identified no apparent intraabdominal source for the free air. Oxygen therapy was initiated. Abdominal exam remained normal and patient had no new complaints. Repeat chest X-ray demonstrated improvement of the pneumothorax but persistence of the pneumoperitoneum. The patient was discharged home and at her 3-week follow up appointment, the pneumothorax had resolved with improvement in volume of pneumoperitoneum present.
Discussion: Pneumoperitoneum is often considered a surgical emergency; however, it is important for hospitalists to be aware of causes that may not require surgical intervention. Loeys Dietz Syndrome is an autosomal dominant connective tissue disorder caused by mutations in TGFβ signaling. First described in 2005 by Drs. Loeys and Dietz, LDS is characterized by four main clinical features including aortic aneurysms, arterial tortuosity, hypertelorism and broad based or bifid uvula. There is phenotypic variation in this syndrome with a spectrum of associated clinical characteristics. Pneumothorax occurs in approximately 5% of patients with LDS, compared to 0.01% in the general population. In addition, LDS has been associated with spontaneous rupture of bowel and spleen.Pneumoperitoneum, in 90-95% of cases, is caused by hollow viscous perforation and represents a surgical emergency. Our patient had no fever, no leukocytosis, no abdominal pain and no peritoneal signs. Furthermore, CT imaging of chest, abdomen and pelvis revealed no abdominal source for the pneumoperitoneum. This case instead represents an example of nonsurgical pneumoperitoneum (NSP) where treatment strategies are conservative rather than surgical. Nonsurgical pneumoperitoneum can be categorized into five groups: postoperatively retained air, thoracic, abdominal, gynecologic and idiopathic. Due to Loeys Dietz Syndrome, the patient had an aortic root aneurysm and 10 years earlier underwent a bio-prosthetic aortic valve replacement and repair of an aortic root aneurysm. The team hypothesized that the pneumoperitoneum was caused by air from the pneumothorax tracking down small defects made from the prior cardiothoracic surgery.
Conclusions: Our case demonstrates an unusual presentation of pneumoperitoneum in a patient with LDS and highlights the importance of recognizing nonsurgical pneumoperitoneum and its relationship with concomitant pneumothorax.