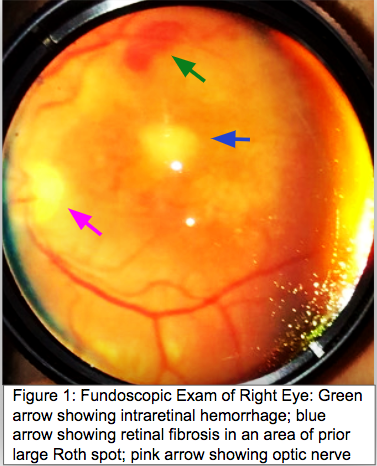
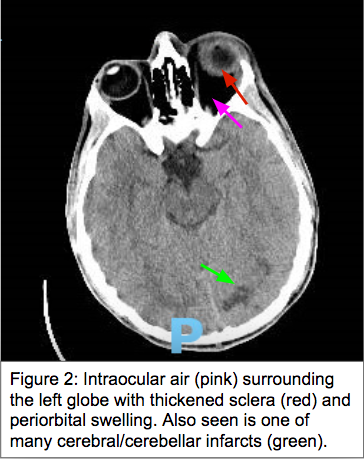
Case Presentation: A 30 year old man with a history of type 1 diabetes mellitus and bioprosthetic aortic valve replacement (AVR) for endocarditis presented with 2 days of left eye pain and vision loss associated with fevers, headache, and nausea. He reported intravenous drug use (IVDU) 4 days prior to admission after 14 months of sobriety in rehabilitation. On admission, he was febrile to 38.7C but hemodynamically stable. He had a loud holosystolic murmur as well as Osler nodes on his toes. Physical exam also revealed a proptotic left eye with cloudy sclera, conjunctival swelling, and minimal light perception. The patient was in diabetic ketoacidosis in the setting of Serratia marcescens bacteremia associated with a large aortic valve vegetation on echocardiogram. Upon ophthalmologic evaluation, he was found to have left eye endophthalmitis requiring urgent intravitreal tap and antibiotics. He eventually underwent left eye enucleation due to persistent infection. Given increasing Roth spots in the right eye with concern for retinal seeding, he also received a right intravitreal tap and antibiotics. Throughout the hospital course, he had evidence of significant embolic phenomena on imaging including multifocal cerebral wedge-shape infarcts, left posterior cerebral artery mycotic aneurysm, and numerous splenic and renal infarcts. Extensive discussions were held between multidisciplinary teams regarding the value and risks of surgical interventions given his AVR due to Rothia mucilaginosa endocarditis associated with IVDU 1 year prior and unclear commitment to maintaining sobriety. The decision was ultimately made to pursue a resternal approach Bentall procedure in which the aortic valve, root and ascending arch were replaced. He remains inpatient for completion of intravenous antibiotics.
Discussion: Infective endocarditis is an infection of the endocardial surface of the heart with prosthetic valves and IVDU being major risk factors. Friable infected cardiac tissue can dislodge and cause distant infarcts or abscesses. Hematogenous bacterial seeding of the eye can result in various ocular manifestations including Roth spots (micro-hemorrhage), vessel occlusion, and rarely endogenous endophthalmitis, wherein the infection involves the vitreous and/or aqueous humors. Only 2–8% of endophthalmitis cases are endogenous, while majority are exogenous in the setting of trauma or eye surgeries. Endogenous endophthalmitis requires both systemic antibiotics as well as intravitreal antibiotic injections and/or vitrectomy (replacement of vitreous humor) to maximize retention of visual acuity. Most cases result in enucleation, or removal of the eye, especially when invasive ocular therapies are delayed. This highlights the importance of maintaining a high index of suspicion for ocular complications in patients with underlying infective endocarditis, liver abscess, or meningitis.
Conclusions: Septic emboli from endocarditis can lead to severe end organ damage, including ocular complications that require early intervention to avoid enucleation. IVDU and prosthetic valves are risk factors for endocarditis, which poses an ethical dilemma when evaluating surgical candidacy for non-native valve replacement. Surgical interventions are often withheld due to technical difficulties posed by reinfected valves as well as futility of high healthcare costs if relapse occurs. In light of the opioid crisis, addiction treatment centers are needed to prevent relapse and recurrent episodes of endocarditis.