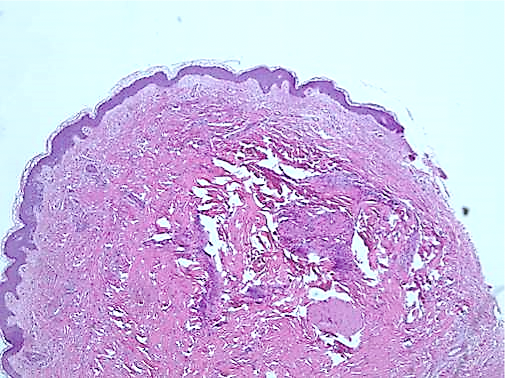
Case Presentation: 65 year old man with history of end stage renal disease, ischemic cardiomyopathy, paroxysmal atrial fibrillation, diabetes presented with complaints of rash in his bilateral legs for four days. Few days later, he noticed petechial rash involving bilateral ankles and feet that started on the left side and did spread to involve bilateral lower extremities primarily anteriorly. He denied any abnormal skin sensation, burning and itching in the involved area initially but later developed these symptoms over a course of few days. No tingling, numbness, pain in the area of the rash, raynaud’s phenomenon, skin ulcers, trauma, loss of hair or tightening of skin. He had been on coumadin for atrial fibrillation but because of excessive ecchymoses he was switched to Eliquis about 6 weeks ago. On examination, he appeared alert with no apparent distress. Vitals were normal. There were few scattered non-tender flat ecchymotic circular lesions measuring less than 1 cm on his left dorsal hand. There were few lesions on anterior knees and shins measuring up to 2 cm in the lower shins from approximately the sock line distally there were coalescing flat to slightly raised non-tender ecchymotic rash. Chemistry panel and complete blood count were normal. Blood cultures were negative.Workup for vasculitis including C3, C4, ANA, ANCA, HIV, HBV, HCV, SPEP, cryoglobulins was negative. He also had diagnostic studies including a nuclear cardiac blood pool MUGA which was not supportive of systemic vasculitis. Right leg skin punch biopsy revealed an inflammatory infiltrate consisting of predominantly neutrophils, with some lymphocytes and scattered eosinophils in small vessels of the superficial and mid dermis consistent with leucocytoclastic vasculitis (LCV). Nuclear dust and extravasated erythrocytes were noted in the interstitium. Scattered eosinophils were noted, which was suggestive of a drug hypersensitivity reaction. Direct immunofluorescence (DIF) revealed granular IgA staining and few C3 clumps in the superficial dermal blood vessels .Based on these findings patient was diagnosed with cutaneous IgA vasculitis. Apixaban was stopped and patient was switched to Warfarin. After topical and systemic prednisone therapy he reported improvement in rash.
Discussion: LCV is defined histologically as a predominantly neutrophilic perivascular infiltrate affecting cutaneous post-capillary venules with fibrinoid deposits in the vessel wall [1]. About 50% cases of LCV are idiopathic while 15%–20% are due to infections, 15%–20% due to inflammatory diseases such as collagen vascular disorders, 10%–15% cases are related to medications and drugs and very few cases are associated with malignancy [1, 2]. Common drugs implicated are penicillins, sulfonamides, quinolones, analgesics, diuretics, anticonvulsants, phenothiazines, allopurinol, and colony-stimulating factors [1].Clinically, it manifests as purpura, urticaria, or ulcers of skin in the dependent areas but other organs can be involved as well [1, 2].
Conclusions: NOACs have been widely used as alternatives to warfarin because of their safety and efficacy. Several cases of rivaroxaban and dabigatran associated LCV have been described in the literature while only few cases have been attributed to apixaban. We emphasize that clinicians should be aware of this rare but important side effect with increasing use of NOACs.