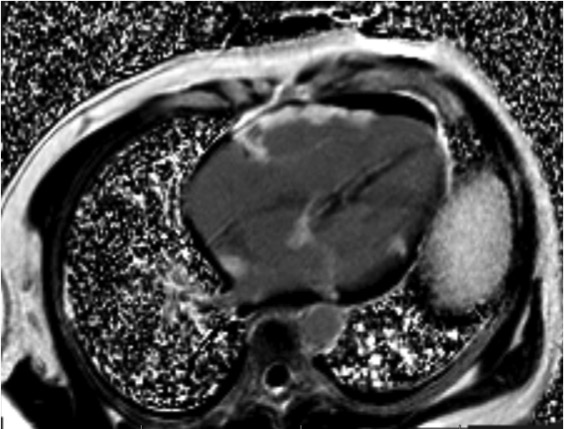
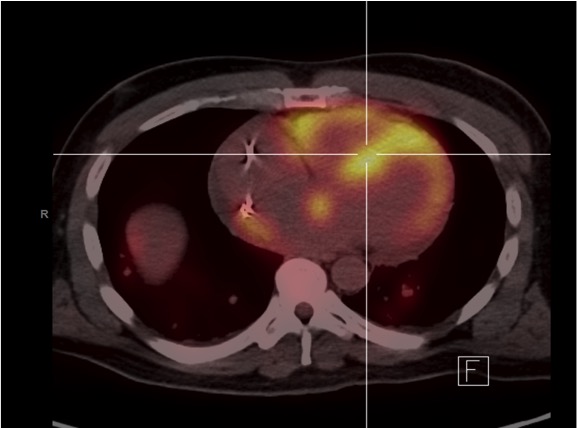
Case Presentation: A 47-year-old African-American man with obstructive sleep apnea presented to the emergency department after being called-back due to evidence of complete atrioventricular (AV) block on routine electrocardiogram. Patient reported a 6-month history of fatigue and exertional dyspnea. On physical examination, he was afebrile and in no acute distress. Vital signs were BP: 142/92 mmHg, HR: 45 bpm, RR: 19/min, and oxygen saturation of 98%. Cardiac examination revealed regular rhythm without murmurs, rubs or gallops. There was no JVD, peripheral edema, and lungs were clear. The electrocardiogram showed AV dissociation with junctional escape rhythm at 48 bpm, poor anterior R wave progression and anterolateral Q waves. Given that patient was hemodynamically stable, urgent temporary transvenous pacemaker was not recommended. Initial laboratory demonstrated high-sensitive troponin T and ESR within normal limits, and CRP-HS mildly elevated at 5.9 mg/dL. Pro-BNP was elevated at 1664 pg/ml. Other laboratory studies were unremarkable. 2D-echocardiogram revealed a left ventricle with ground-glass appearance, concentric hypertrophy, reduced systolic function with EF: 30–35%. Chest imaging was remarkable for cardiomegaly, mediastinal and bilateral hilar lymphadenopathy. Given a young Afro-American patient with no history of ischemic heart disease presenting with an unexplained third-degree AV block, hilar lymphadenopathy and abnormal echocardiogram, the possibility of cardiac sarcoidosis was raised. Gadolinium-enhanced cardiovascular MRI demonstrated extensive biventricular abnormal delayed enhancement with patchy area of abnormal enhancement in a non-vascular distribution mainly at the mid myocardium and epicardium. 18F-fluorodeoxyglucose-positron emission tomography showed an increased biventricular tracer uptake as well as in mediastinal and hilar lymph nodes. At this time, patient with “probable” cardiac sarcoidosis, but tissue biopsy was needed to establish a “definite” diagnosis. However, lung and cardiac biopsies were non-diagnostic. During admission, patient underwent dual chamber implantable cardioverter-defibrillator placement for pacing as well as primary prevention of sudden cardiac death, and was started on medical therapy for heart failure and prednisone for sarcoidosis.
Discussion: Sarcoidosis is a multi-system disease of unknown etiology characterized histopathologically by noncaseating granulomas in involved tissues. The lungs are affected in over 90% of patients. Nevertheless, up to 30% of patients can present with extrapulmonary disease. Cardiac involvement has been described in 5% of patients with sarcoidosis. When the heart is involved, its presentation can vary from an incidental discovery to a patient with heart failure and sudden death.
Conclusions: Cardiac sarcoidosis is a challenging diagnosis, thus under-recognized. It commonly presents with conduction abnormalities, being AV block the principal manifestation. This case illustrates the need for high clinical suspicion and integration of multiple advanced cardiac imaging studies for the diagnosis of cardiac sarcoidosis in patients <60 years who present with unexplained third-degree AV block. Multiple modalities of cardiac imaging helped us made the diagnosis promptly, start proper therapy, and possibly improve his survival.