Background: The use of early warning systems (EWS) to augment clinical care is of increasing interest with recent publications showing EWS algorithm alerts coupled with clinical response actions to have significant morbidity and mortality benefit.1 At Stanford Hospital we are developing an alert and response EWS using a machine learning (ML) model predicting clinical deterioration to identify patients at risk of imminent decompensation and employ pre-emptive intervention. This retrospective cohort study aimed to understand the cases identified by the ML model which experienced an acute decompensation in order to better design our clinical response intervention. In contrast to other recent EWS systems2,3 we analyzed the etiologies of decompensations that were identified (eg hypoxia, shock, etc.) and the generalizability of the model to all specialty services.
Methods: The ML model, known as the Clinical Deterioration Index (CDI) was developed by Epic Systems (Verona, WI) and incorporates 30 variables including vital signs, demographic data, and nurse charting into a linear regression model trained to identify patients at risk of decompensation within 24 hours. The algorithm was run every 15 minutes, flagging a patient if identified to be at risk. We retrospectively analyzed all acute decompensation events (rapid response codes) at Stanford Hospital from February to May of 2020, assessing for the presence of a CDI flag, etiology of decompensation, primary service, and mortality.
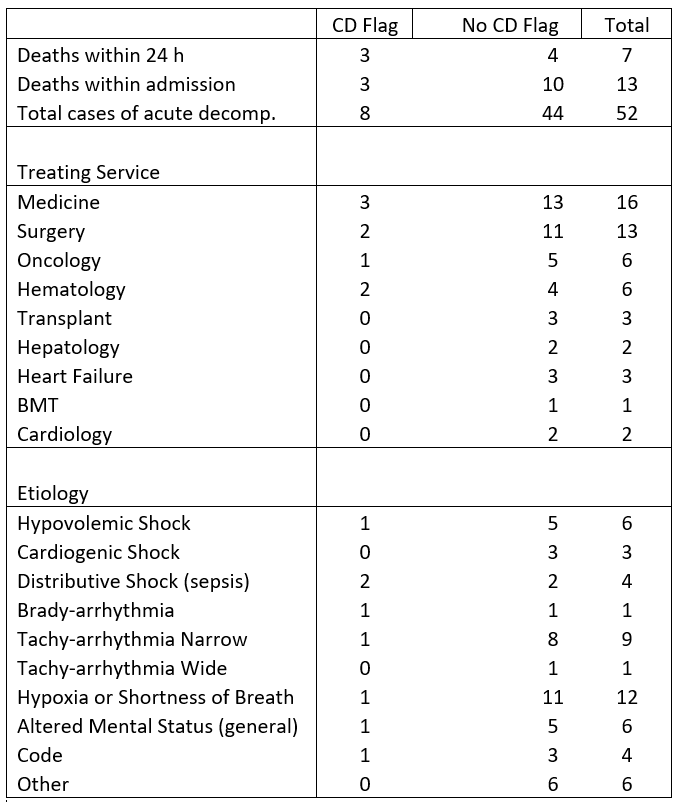
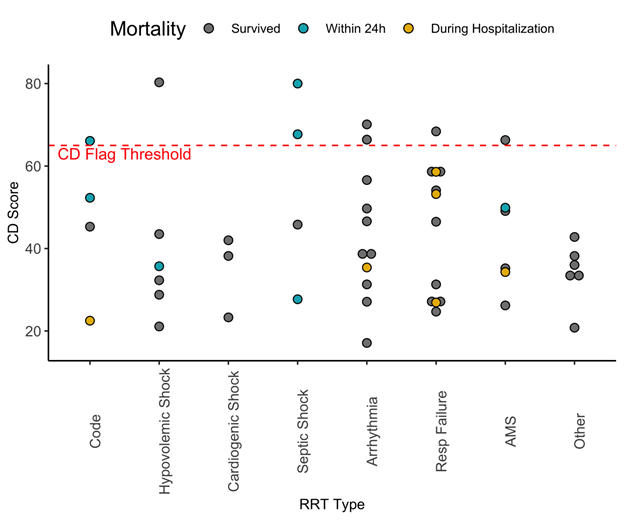
Results: The CDI identified 8 of 52 patients who experienced an acute decompensation during the study period. Mortality within 24 hours was 38% in patients with a decompensation and CDI flag compared to 9% in decompensations without a flag (p value 0.06). The ranges of CDI scores and rates of flagged acute decompensations were well distributed without obvious skew towards specific decompensation etiologies (see Figure 1). The model identified decompensations of medical, hematology, oncology, and surgical specialty patients. Acute decompensations of subspecialty services were less common (Table 1).
Conclusions: In this small sample size of early data, presence of a CDI flag trended towards increased mortality among patients who decompensated and were flagged by our algorithm. Although this was not a significant predictor (p value 0.06) of 24-hour mortality, we are confident that as we continue to collect data this result will become significant. The model was applicable to all common etiologies of acute decompensation and identified patients from both medicine and surgical specialties. Ultimately our findings will better guide efforts in developing the intervention arm of our EWS by identifying potential clinical intervention targets.