Background: Hospitalists play an essential role in educating residents on inpatient rotations. One critical way to ensure the success of trainees is to provide timely feedback and written evaluations, which may be difficult amidst conflicting tasks. Hospitalists face additional challenges with the large volume of learners to supervise, and with irregular resident schedules and frequent team changes which disrupt the attending-resident continuity needed for meaningful feedback. In our hospitalist division, these issues were exacerbated by our cumbersome resident evaluation process: attendings would list resident feedback in a common Word document, which was then transferred by the ward rotation directors into a standardized New Innovations (NI) form under a common account. In AY 2017-18, 0% of pediatric residents received a written evaluation within 14 days after completing their inpatient rotation (19% returned <30 days, average return time=36 days) and 50% of residents never received an evaluation, meaning half returned to the rotation without the opportunity to be aware of and correct key deficiencies. The aim of this project was to use a series of interventions to improve completion rates of resident inpatient evaluations returned <30 days from 19% to 50% and the average return time from 36 days to <30 days post-rotation over 6 months. The balance measure was the amount of administrative time required to meet this aim.
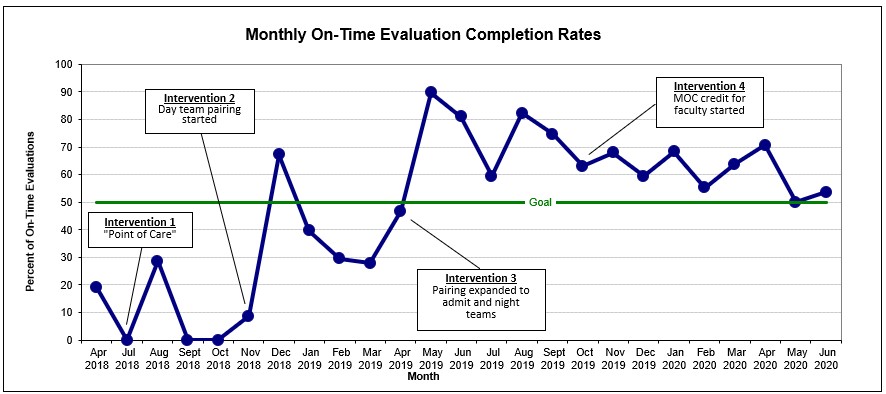
Methods: Intervention 1: Residents were tasked with initiating “point-of-care” feedback and documentation from attendings via NI. Intervention 2: Each hospitalist was provided a personal NI account and an administrator paired each hospitalist with his/her residents for the week. Hospitalists received automatic reminders from NI with direct links to their residents’ evaluation forms, to be completed on a computer or mobile device and instantly released to the resident. Batched comments were sent to the ward rotation directors to be included in summative rotation evaluations. Intervention 3: Paired admit and night team residents and attendings. Intervention 4: This QI project was accepted by the institution’s Maintenance of Certification (MOC) governance committee to offer Part 4 credit to hospitalists who met thresholds for timely completion evaluations.
Results: Intervention 1 was unsuccessful and resulted in lower rates of evaluation return. The combinations of Interventions 2 and 3 were very effective as faculty consistently met the threshold of returning at least 50% of assigned evaluations within 30 days post-rotation (67% returned <30 days, average return time=18 days), starting May 2019 (Figure 1). The incentive of MOC credit further sustained this improvement. After the initial learning curve, the administrative time spent was 1 hour per week to complete the pairings and 5 hours every 6 months to assess MOC credit. Faculty have found this new system quick and easy to use, and residents and program directors have valued the copious, robust feedback.
Conclusions: We developed a system that enabled hospitalists to complete resident rotation evaluations in a timely manner with minimal administrative and hospitalist burden, and further incentivized faculty with MOC Part 4 credit. This process can be utilized by hospitalists across institutions and specialties, with thresholds modified to further improve evaluation metrics.