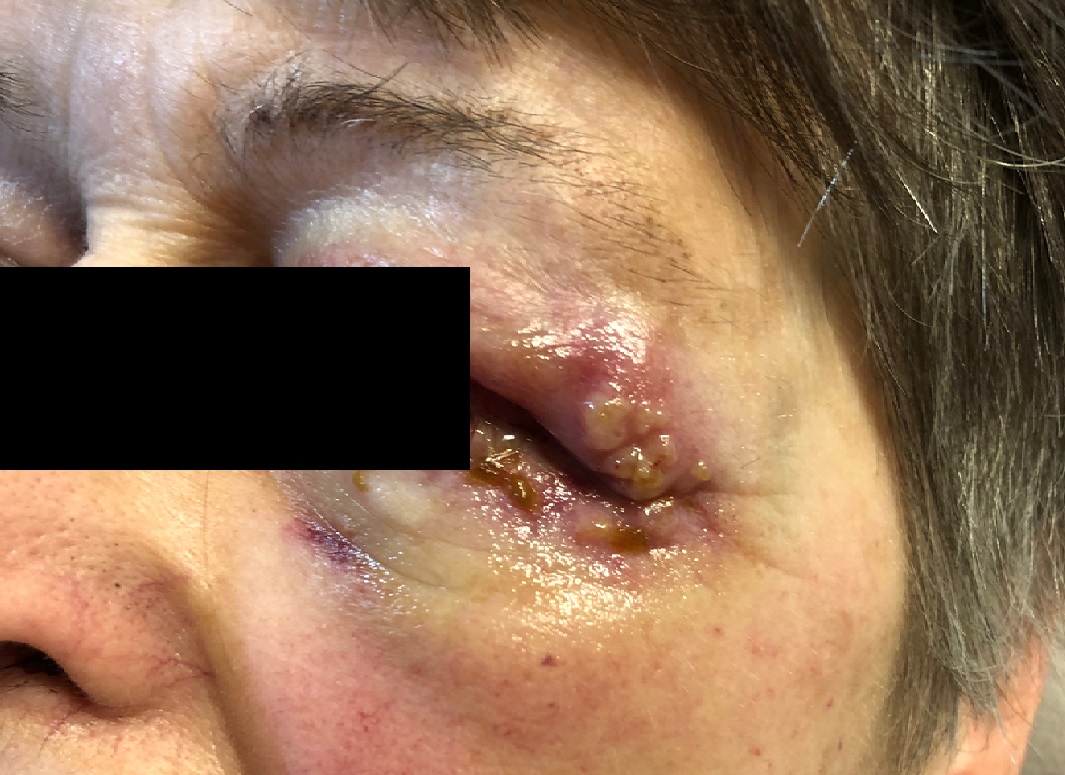
Case Presentation: A 72-year-old female never-smoker was admitted for progressive dyspnea, pleuritic chest pain, and non-productive cough after failing outpatient treatment for presumed community-acquired pneumonia based on chest x-ray findings. On arrival, she was afebrile, hemodynamically stable, and breathing comfortably on room air. Physical exam revealed pulmonary crackles and a clean-based ulcer on the lateral tongue border. Initial labs showed neutrophil-predominant leukocytosis, normocytic anemia, elevated inflammatory markers, and creatinine over four times her baseline. Urinalysis showed proteinuria and hematuria without dysmorphic red blood cells or casts. CT chest showed infiltrative mass-like consolidations in both lung bases with innumerable peri-bronchovascular nodules. Given the multiorgan involvement, rheumatological workup was done and showed myeloperoxidase and perinuclear anti-neutrophil cytoplasmic antibody (ANCA) positivity with mildly elevated rheumatoid factor and antinuclear antibodies. Confirmatory renal biopsy showed pauci-immune necrotizing and crescentic glomerulonephtiris with necrotizing arteritis, and broncheoalveolar lavage showed hemosiderin-laden macrophages without signs of infection or frank bleeding. Before starting immunosuppression, an infectious work up was done, including hepatitis panel, fungal mycoses, HIV, CMV, EBV, sputum and urine culture, and quantiferon assay. She was started on pulse-dose steroids. Despite starting steroids, her oral ulcers progressed to other areas of the oropharynx (Image 1). She also developed nasal crusting with dried blood seen in both nasal cavities on flexible laryngoscopy. Concomitantly, she developed painless periorbital vesicles with erythema, edema and mattering around the eyes (Image 2). This progression raised concerns for an infection, especially with planned chronic immunosuppression. These lesions were cultured and biopsied, and broad spectrum antibiotics were started. Tongue biopsy was consistent with ANCA-associated vasculitis (AAV), showing ulceration, necrosis, and inflammation, but no definitive stigmata of vasculitis were present. Skin biopsy showed neutrophilic inflammation and small-vessel fibrinoid necrosis, further supporting the diagnosis of AAV. With infection ruled out, antibiotics were discontinued, and the patient was discharged on immunosuppression.
Discussion: Pulmorenal syndrome is typically caused by autoimmune processes like AAV, anti-glomerular basement membrane disease, and systemic lupus erythematosus, and depending on the cause, other systemic findings may be present. In AAV, cutaneous manifestations are among the least likely and may appear similar to infection that would need treatment prior to starting immunosuppression. Although initial treatment for autoimmune pulmorenal syndrome is similar regardless of etiology, AAVs are likely to recur and require chronic immunosuppression, often with rituximab. In this case, ruling out infection was important given the potential sight risk with periorbital involvement and the risk of infection in the oropharynx.
Conclusions: In high-risk areas like the oropharynx or the orbit, infection must be ruled out prior to starting chronic immunosuppression for prevention of ANCA-associated vasculitis recurrence. Multiple diagnostic modalities may be necessary to differentiate between infection and manifestations of AAV.