Background: Nearly half of hospitalized patients with bacteriuria or treated for pneumonia receive unnecessary antibiotics (non-infectious/non-bacterial syndrome, e.g., asymptomatic bacteriuria), excess duration (antibiotics prescribed for longer than necessary), or avoidable fluoroquinolones (safer alternative available) at hospital discharge.1-3 However, it is unknown whether antibiotic overuse at discharge varies between hospitals or is associated with patient outcomes.
Methods: From 7/2017-12/2018, trained abstractors at 46 Michigan hospitals collected detailed data on a sample of adult, non-intensive care, hospitalized patients with bacteriuria (positive urine culture with or without symptoms) or treated for community-acquired pneumonia (CAP; includes those with the disease formerly known as healthcare-associated pneumonia [HCAP]). Antibiotic prescriptions at discharge were assessed for antibiotic overuse using a previously-described, guideline-based hierarchical algorithm.3 Here, we report the proportion of patients discharged with antibiotic overuse by hospital. We also assessed hospital-level correlation (using Pearson’s correlation coefficient) between antibiotic overuse at discharge for patients with bacteriuria and patients treated for CAP. Finally, we assessed the association of antibiotic overuse at discharge with patient outcomes (mortality, readmission, emergency department visit, antibiotic-associated adverse events) at 30 days using logit generalized estimating equations adjusted for patient characteristics and probability of treatment.
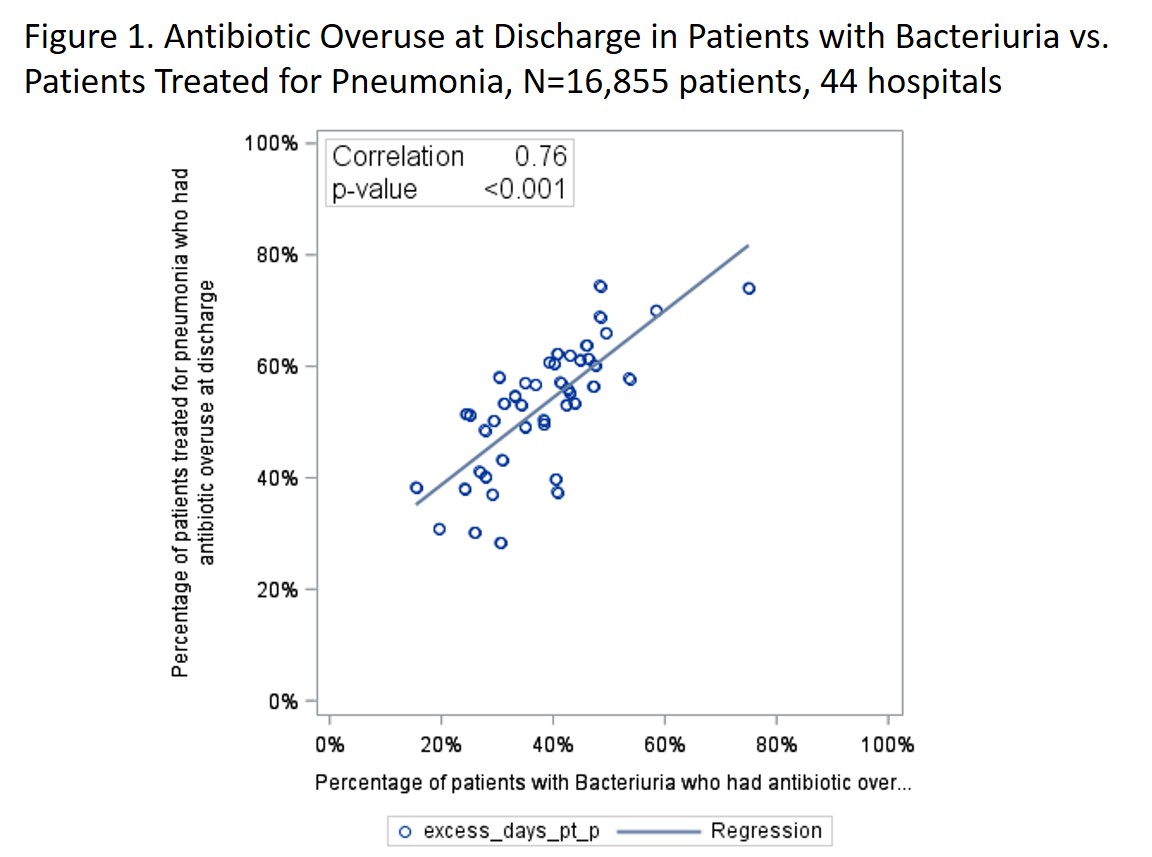
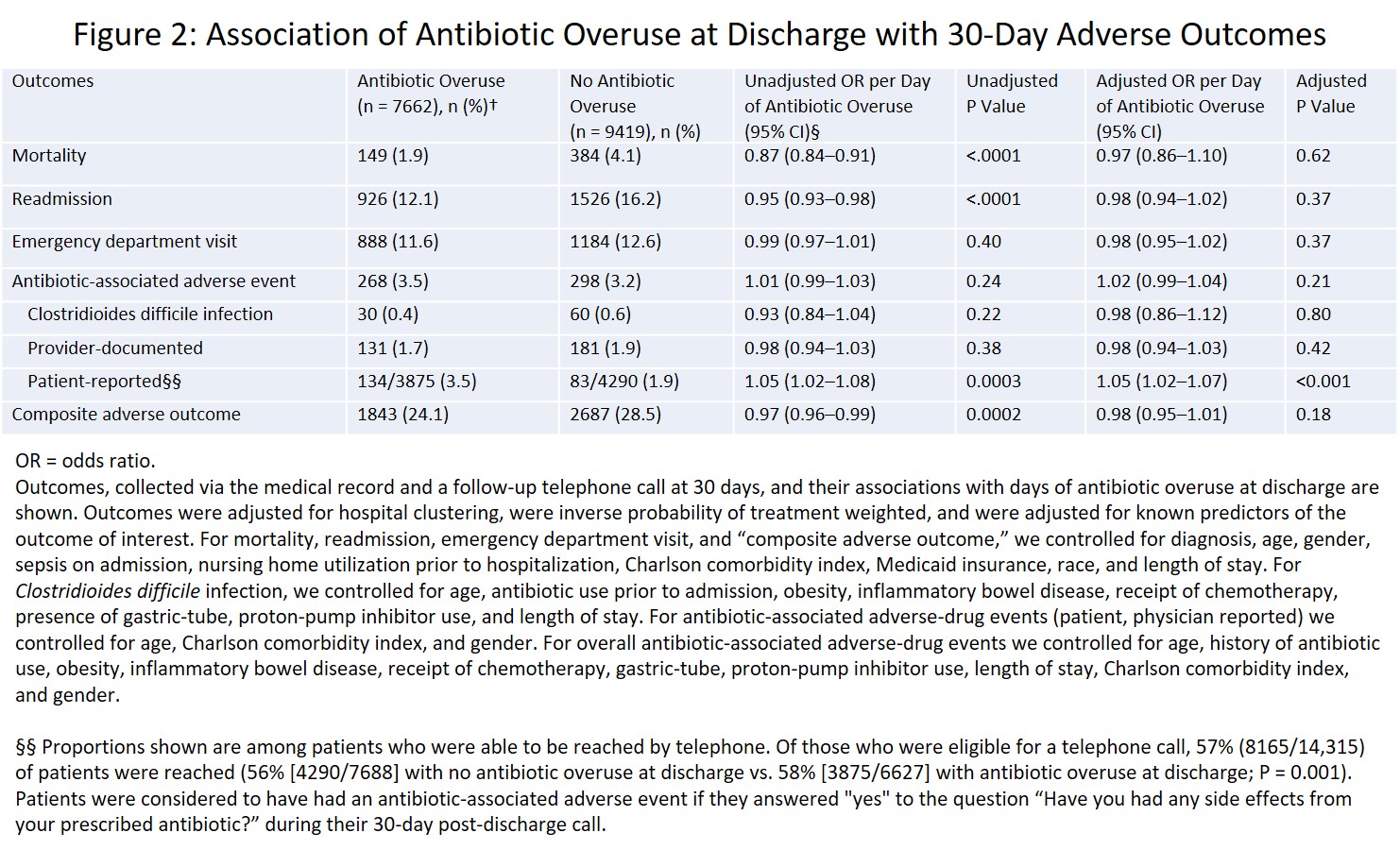
Results: Of 17,081 patients (7,207 with bacteriuria; 9,874 treated for pneumonia), nearly half (42.2%) had antibiotic overuse at discharge (36.3% bacteriuria, 51.1% pneumonia). The percentage of patients discharged with antibiotic overuse varied five-fold among hospitals (from 14.7%, 95% CI: 8.0-25.3%, to 74.3%, 95% CI: 64.2%-83.8%). Hospital rates of antibiotic overuse at discharge were strongly correlated between bacteriuria and CAP (Pearson’s correlation coefficient=0.76, P=<0.001; Figure 1). In adjusted analyses, antibiotic overuse at discharge was not associated with death, readmission, emergency department visit, or Clostridioides difficile infection. However, each day of overuse was associated with a 5% increase in the odds of patient-reported antibiotic-associated adverse events after discharge (Figure 2).
Conclusions: Antibiotic overuse at discharge was common, varied widely between hospitals, and was associated with patient harm. Furthermore, antibiotic overuse at discharge was strongly correlated between two disparate diseases, suggesting that prescribing culture or discharge processes—rather than disease-specific factors—contribute to overprescribing at discharge. Thus, discharge stewardship may be needed to target multiple diseases.