Background: Venous thromboembolism (VTE), including deep vein thrombosis and pulmonary embolism, is a serious public health problem causing over 90,000 deaths each year. VTE rates at our institution have been high and costly, with insurer penalties for post-operative VTE exceeding $5.5M in 2014. While prophylaxis for at-risk inpatients can reduce hospital-associated (HA) VTE by up to 65%, only about 60% of surgical inpatients and 40% of medical inpatients receive appropriate VTE prophylaxis. Previous quality improvement (QI) efforts to reduce VTE rates at our institution have relied largely on retrospective billing data, and no standardized protocol currently exists for data collection and analysis.
Purpose: To reduce HA-VTE rates through an innovative QI process that leverages novel data analytics tools and Bowtie risk analysis methodologies used in the airline traffic control and nuclear energy industries.
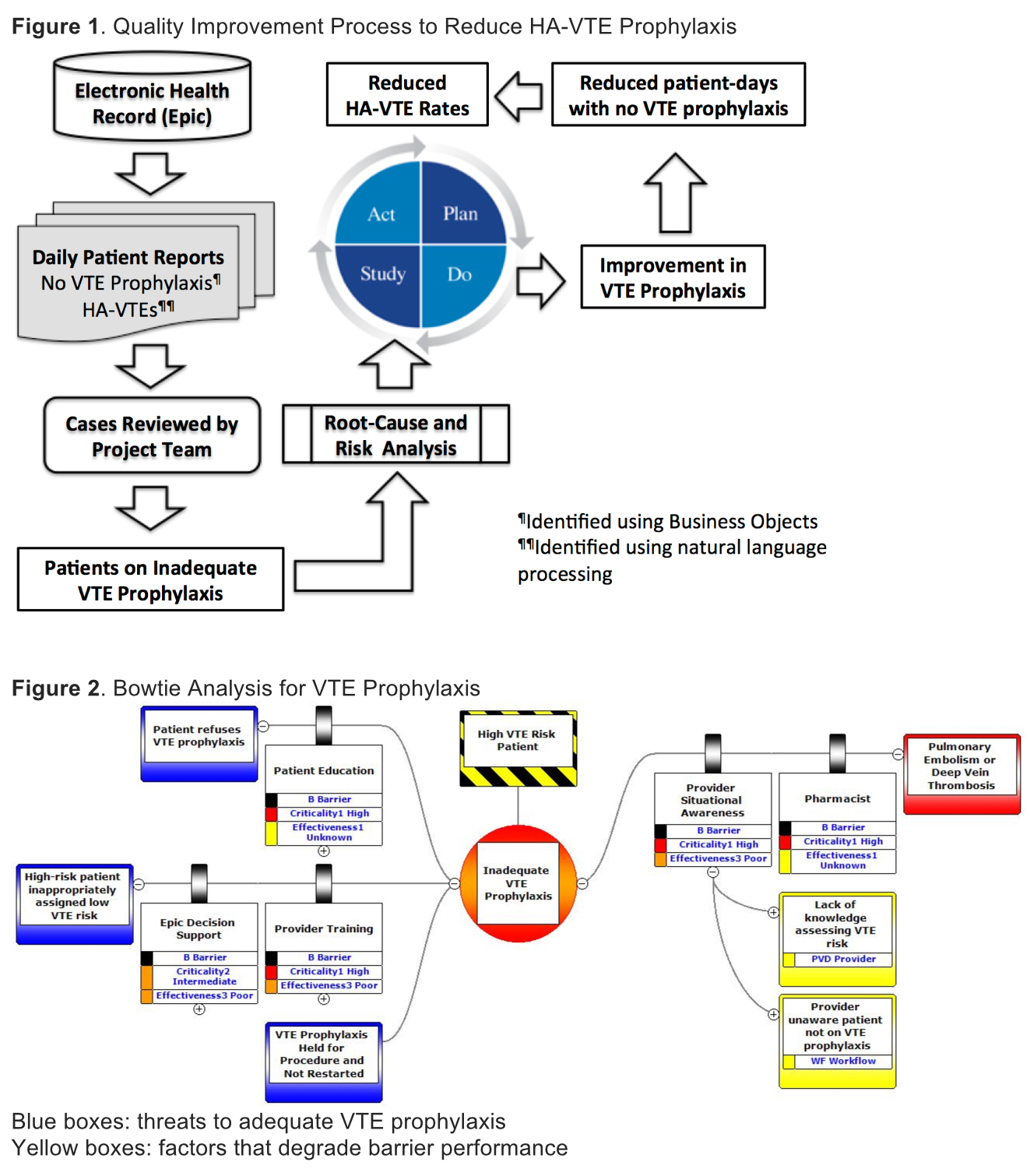
Description: Our new QI process utilizes data analytics and informatics tools, that are integrated with our electronic health record (EHR), including natural language processing (NLP), to derive insights from EHR data by identifying acute HA-VTE events and hospitalized patients not on VTE prophylaxis (figure 1) in near real-time. Identification of each HA-VTE event or high-risk patient not on VTE prophylaxis triggers a concurrent root-cause and risk analysis (RCA) by the QI project team while patients are still in the hospital and providers readily available for interviews. The project team meets weekly to review RCA data in order to develop and refine the Bowtie risk analysis (figure 2) that will inform Plan-Do-Study-Act (PDSA) cycles designed to improve VTE prophylaxis.
Conclusions: Our new QI process is being piloted on the hospitalist service and our Bowtie analysis has identified 3 primary threats to evidence-based VTE prophylaxis: 1) high-risk patients inappropriately assigned to low VTE risk category by providers, 2) VTE prophylaxis held for operative procedures and not restarted, and 3) high-risk patients refusing VTE prophylaxis. We are currently developing interventions (e.g., refining our EHR decision support) to improve VTE prophylaxis based on findings from our Bowtie analysis (figure 2). Future QI efforts include expanding and scaling our novel approach to other quality and safety measures.