Background: Design thinking is a framework for creative problem solving. When the design thinking process (often leveraged in fields outside of healthcare delivery) is applied, it leads to a human-centered path to innovation. The infusion of deep empathy, holistic examination, inclusive collaboration, and effective iteration fosters sustainable solutions for complex human concerns. In traditional problem-solving, upon defining the problem, emphasis is placed on assessing the best solution from an inadvertently limited set of choices. In design thinking, however, for a given issue, focus is placed on identifying all the gaps and unmet human needs to define a problem comprehensively and empathically. Thereafter, a variety of ideas are rapidly tested and iterated upon to discover the best targeted solution. For this project, as caregiver burden remains a dire concern in healthcare and public policy discourse, heightened by the COVID-19 pandemic, we sought to use design thinking methodologies to gather insights on how to support caregiver-patient-hospitalist relationships to enhance patients’ experience during their hospitalization and with transitions in their care.
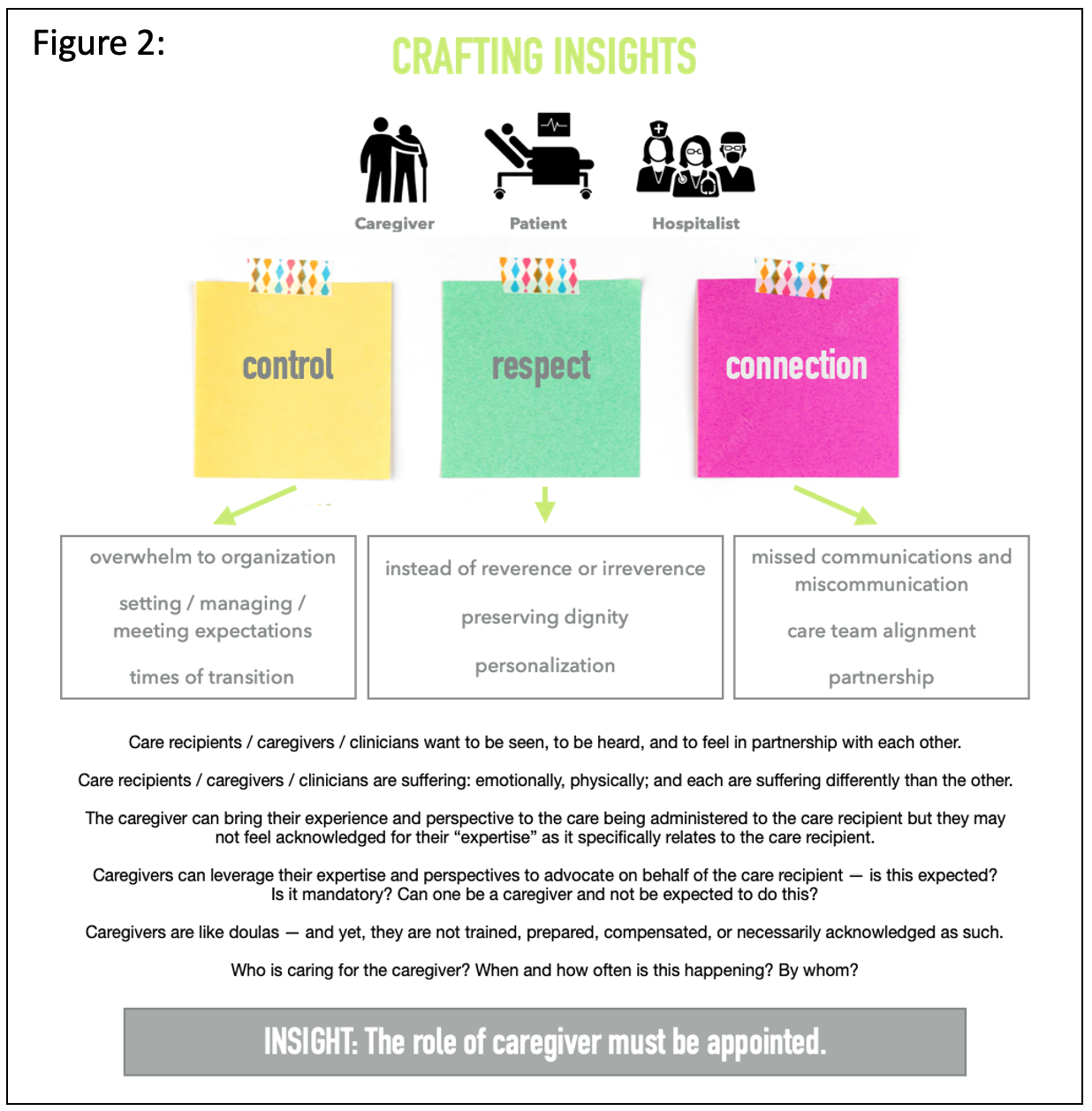
Purpose: Using the global design and innovation company, IDEO’s system for crafting insights for innovation (1) we focused on the first two components of the Stanford d.school’s design thinking paradigm (2) – Empathize and Define – to identify opportunities to address caregivers’, patients’, and hospitalists’ comprehensive needs in service of the hospitalized patient’s total experience.
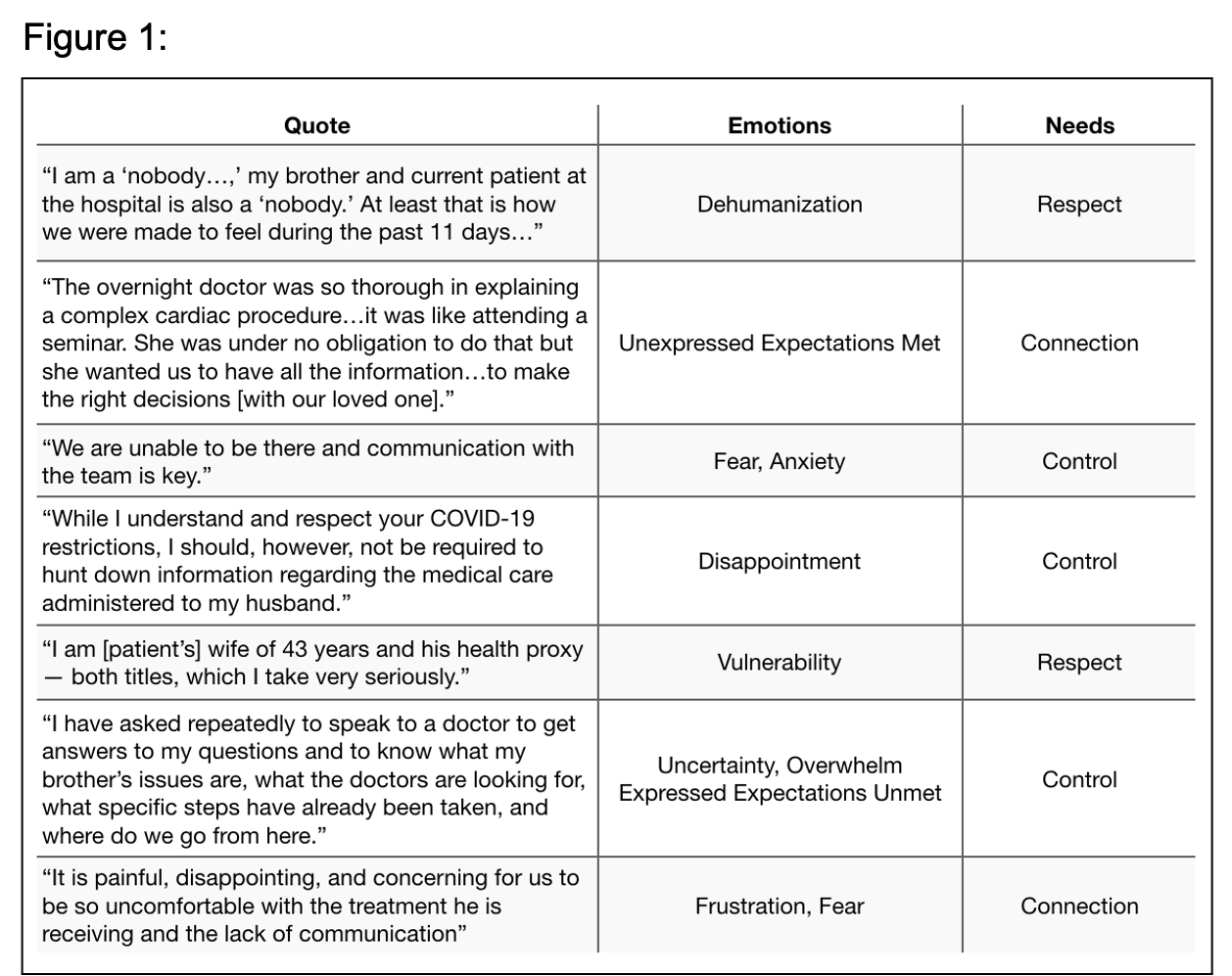
Description: Stakeholder participants (caregivers, patients, hospitalists) were engaged in a human-centered design process through observation, interviews, and a practical empathy experience. In the observation phase direct and asynchronous moments of caregiver interaction with hospital care teams were evaluated via time spent with unit clerks fielding phone calls and through a review of grievance letters sent. Notably, the gaps exposed regarding communication (especially given visitation restrictions in the pandemic) and the extrapolated needs of caregivers (Fig 1) matched those identified in open-ended interviews conducted with hospitalists. Both caregivers and hospitalists expressed common values of respect, connection, and control. To round out our examination and immerse ourselves in the authentic experience of a hospitalized patient, we recreated their journey from arriving in the emergency room to transport to a medical bed after admission to preparation for discharge. Allowing our senses to become tools, this physical journey through the hospital enabled further insight into the complexity and frequent isolation of this experience.Armed with these stories and learnings from real people and subsequent informed conclusions, the process of crafting insights was revealing (Fig 2). Our final, succinct summary insight: “The role of caregiver must be appointed,” unifies each party’s behaviors, emotions, needs, and values and their poignant and significant, tripartite relationship. This insight builds focus and shared motivation towards optimizing the hospitalized patient’s care and experience.
Conclusions: Design thinking empowers hospital medicine to expand on our strengths of process and quality improvement, leveraging our empathy and relationship-centered communication skills from patient care to be natural facilitators of innovation able to creatively address a diversity of challenges in acute healthcare delivery.