Background: Lack of academic productivity poses barriers to the promotion of hospital medicine faculty members at academic medical centers.1,2 New faculty members may face additional challenges with academic promotions due to lack of research productivity and availability of career mentors. Lack of academic funding for early career academic hospitalists has previously been highlighted as a barrier for promotion for faculty pursuing clinician-researcher careers.3
Purpose: The goal of the Johns Hopkins Division of Hospital Medicine Innovation Grant program is to identify innovative academic projects that would improve the division’s academic profile. It provides seed funding for faculty to develop their interests and create a portfolio of work that can subsequently be used for larger grant applications.
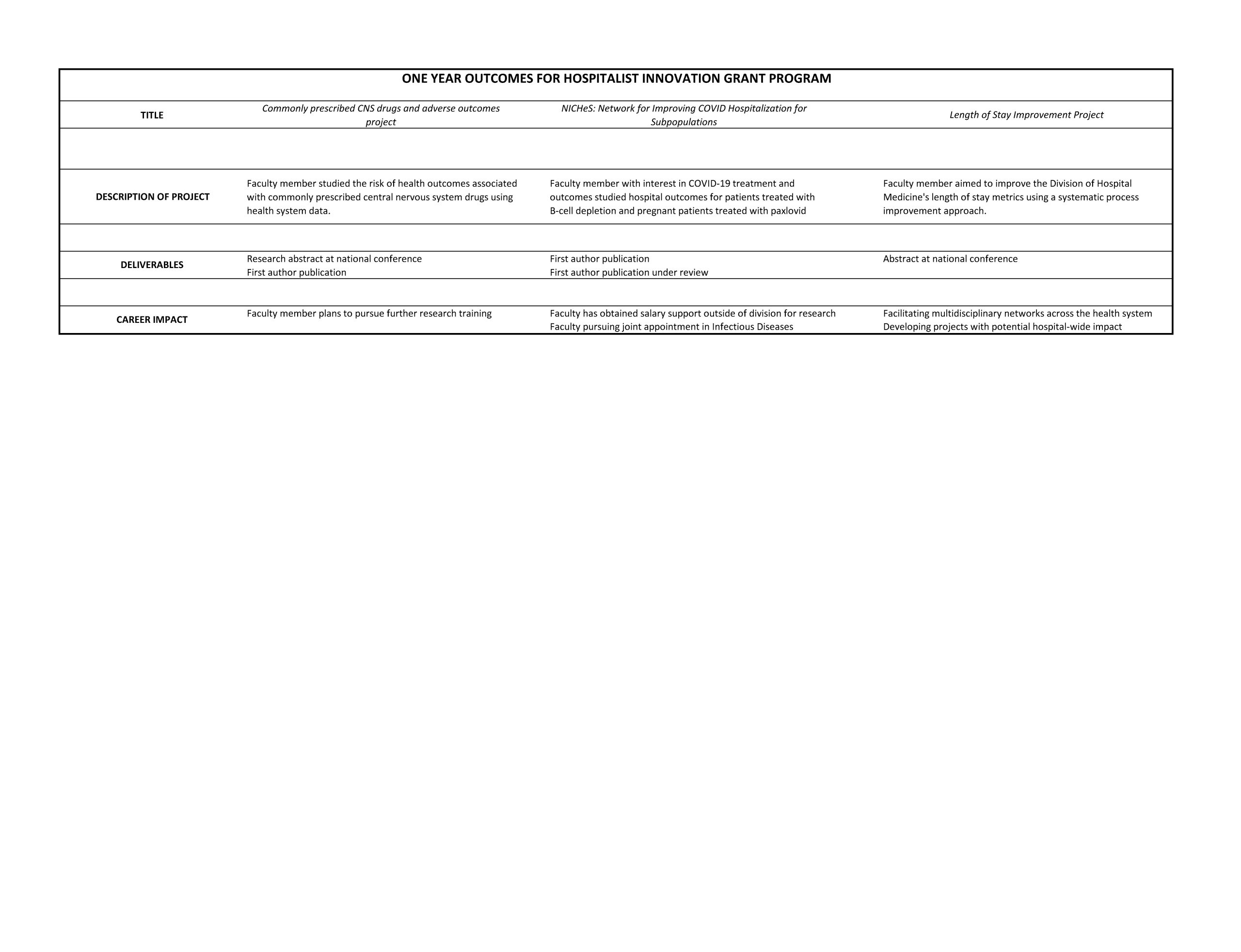
Description: The Johns Hopkins Division of Hospital Medicine launched the Hospitalist Innovation Grant program in 2021. The program is funded with $75,000 annually and can be used for salary support in addition to other project related costs. These funds are provided via philanthropic gifts to the Division of Hospital Medicine as well as consulting engagements. Prior funding mechanisms within the division could only be used for direct costs such as publication fees, conferences, and access to research assistants.Applicants develop a proposal including a background, specific aims, key deliverables, roles and key stakeholders, as well as a budget and timeline. These proposals are reviewed by hospital medicine leadership and proposals are then presented to the entire division at a faculty meeting for feedback after which decisions are made regarding funding. The program has funded three projects thus far. One scholar studied the adverse outcomes of commonly prescribed central nervous system drugs, achieving a national-level abstract competition award and a first-author original research publication. Another faculty member has pursued research in COVID-19 clinical outcomes developing a research program called NICHeS (Network for Improving COVID Hospitalization for Subpopulations). The faculty member has several research studies in vulnerable populations leading to an accepted first author publication and one in review.A third faculty member received funding to develop interventions to reduce length of stay (LOS) within the hospitalist division. One intervention has been to create an interdisciplinary tracheostomy team to improve outcomes for this patient population. The work has been featured in an abstract at a national quality improvement conference.
Conclusions: The Innovation Grant program has supported faculty members who are committed to developing their academic portfolio. While the funding mechanism may not be replicable in all settings, the program may serve as an example of an approach to developing structures to fund and promote career development with relatively modest funding support. The innovation also addresses a key barrier for early career hospitalists engaged in research who lack training opportunities such as T32 or similar funding mechanisms for early clinician-researchers. Hospital medicine divisions often have relatively few established R-funded researchers who may train and mentor new faculty members. To that end, this newly launched program shows promise in promoting grant writing experience, fostering publications, and provides critical early institutional support for junior faculty.