Background: Disruptions in normal life routines (such as sleep, function, nutrition, etc.) that commonly occur as part of routine hospital care may be traumatic for acutely ill patients and lead to a generalized condition of high risk after discharge that has been described as “post-hospitalization syndrome.” We created the ARCHES cohort study to measure these disruptions in life routines and characterize their impact on post-discharge outcomes of care.
Methods: This is a prospective, longitudinal cohort study of patients (age 50 or older) admitted to a major academic medical center from Dec 2015-May 2017. Exclusion criteria were inability to provide consent in English, observation status, ICU admission, homelessness or active incarceration (prisoners). All patients were enrolled within 24 hours of admission. Validated survey instruments were used for all assessments. A comprehensive assessment of normal life routines was administered on day 1 and repeated at pre-specified intervals. A focused subset of questions was repeated daily until the day of discharge (max 10 days); other assessments are repeated at 1, 3, 6 or 12 months after discharge.
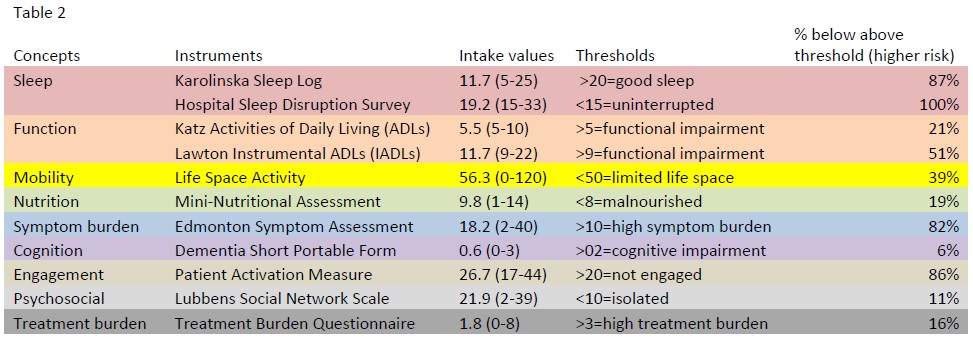
Results: We enrolled 75 patients: average age 65.5, average length of stay 4.8 days, 61% White, 49% Female, 53% Medicare, readmitted patients were not different from non-readmitted patients (Table 1). At the time of admission (baseline), most patients (86.5%) reported poor sleep but good function (21% with any impairment) and nutrition (19% malnourished). Most patients (82%) reported high symptom burden and most (86%) felt un-engaged in their care. Sleep remained poor during hospital stay with 100% of patients reporting hospital-specific disruptions (labs, meds, vitals) as significant disruptions beyond their symptoms. Although levels of symptom burden improved (overall decrease from 18.2 to 15.7, p<0.05) from admission to discharge, levels of engagement remained poor (no significant change) and function worsened (overall change from 5.5 to 7.3, p<0.001). Patients who were readmitted within 30 days were more likely to have higher symptom burden at discharge (increase from 18.1 to 21.3, p<0.1) but were not different in terms of function, sleep, or engagement.
Conclusions: Disruptions in normal life routines during hospitalization such as sleep and function were common in a cohort of older adults; low perceived engagement in care and high symptom burden were also common. Of these factors, only high symptom burden was more common among readmitted patients.
.jpg)