Background: In-hospital cardiac arrest (IHCA) is an unpredictable, catastrophic event affecting approximately 200,000 US adults annually. Best outcomes during IHCA result from focused training and credentialing by AHA (ACLS, BLS). Although hospitalists supervise IHCA, best practices for resuscitation skills, preparedness, plus overall approach remain undefined.
Methods: We developed an online survey of IHCA resuscitation responsibilities for practicing hospitalists. Questions included demographics, physician preparation, and perceptions of IHCA. We assembled a convenience sample of hospital medicine program leads at Veterans Affairs (VA) and non-VA sites throughout the US. Leaders were asked to distribute an electronic survey link to hospitalist physicians at their site. Participants were sent two reminder emails one week apart.
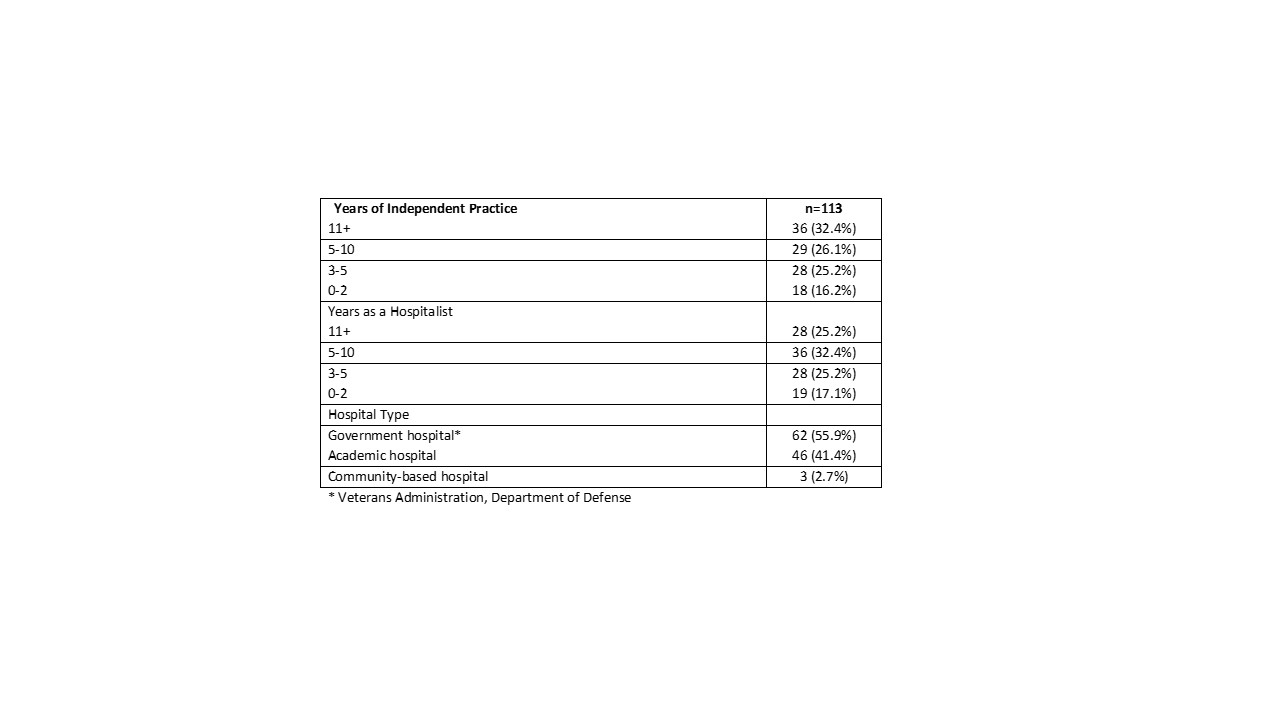
Results: Eleven service Chiefs distributed the survey to 308 hospitalists; 113 hospitalists completed the survey, (37 % response rate). Respondent demographics are detailed in Table 1. Description of responsibilities, training, and thoughts regarding ACLS are detailed in Table 2. Median annual IHCA events reported was 7 (0 to 301). Thirty-five percent of respondents reported completing training beyond Advanced Cardiac Life Support (ACLS) with case simulation (66.7%) and lecture (38.5%) the most common modalities of learning outside of ACLS. Of skills thought to be most important in supervising IHCA, skilled communication was highest at 55.5%, followed by response time (20%), and rapport with staff (12.7%). Of respondents with two years or less of experience, 39% indicated they would voluntarily give up IHCA responsibilities, compared to 69.4% of those with ≥5 years experience (p = 0.04). When asked which medical specialty managed IHCA best, 58% indicated hospital medicine, 38% pulmonology/critical care , and 4% chose emergency medicine. Yet, 75% of participants felt IHCA supervision should be a core competency for hospital medicine.
Conclusions: Hospitalists in this national survey reported being prepared for IHCA and that hospital medicine is the specialty best suited for the role. Future studies are necessary to incorporate qualitative and in-depth measures to inform policy and practice regarding roles in supervising IHCA.
.jpg)
