Background: Hypertensive crisis is classified as either hypertensive emergency or hypertensive urgency, distinguished by presence or absence of end-organ damage, respectively. Guidelines recommend treating hypertensive emergency with intravenous (IV) antihypertensive medications for immediate blood pressure reduction. On the other hand, management of hypertensive urgency involves gradual reduction of blood pressure over hours to days using oral agents. Despite these recommendations, both crises are often reflexively treated in the same way using IV agents. This aggressive treatment for hypertensive urgency is costly and can result in harm to patients.
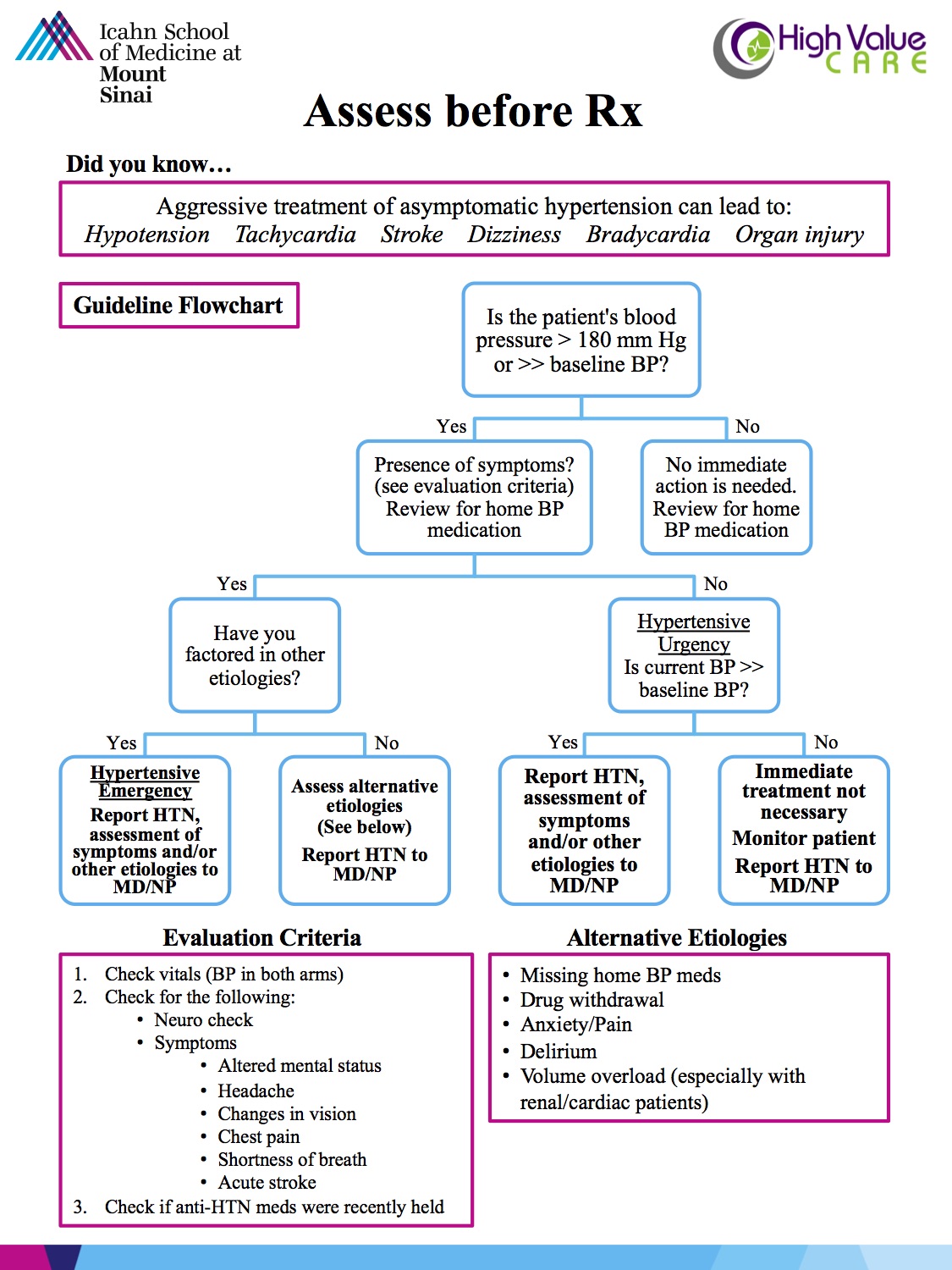
Purpose: We aim to reduce the number of one-time orders of IV antihypertensives that are not indicated for hypertensive urgency. Our goal is to create a culture change that has all members of the care-team “Assess Before Rx.”
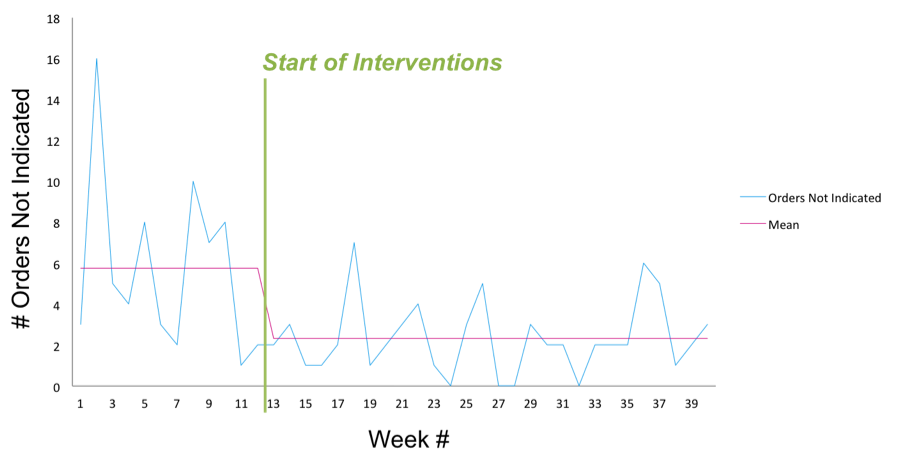
Description: This quality improvement project was initiated on two inpatient medicine units at an urban, tertiary academic medical center. Medical-student led, interdisciplinary interventions were utilized. They included nurse education using fliers and huddle presentations, utilizing the project slogan, “Assess before Rx.” Advanced practitioners and residents were given bi-weekly educational emails. Targeted feedback emails were provided to clinicians when non-indicated IV orders were made. Additionally, electronic medical record advisory warnings were placed on IV antihypertensive orders. We compared pre-intervention data (January – July 2016) to post-intervention (March –September 2017). Data were obtained from utilization reports of labetalol and hydralazine, and retrospective chart review.
Conclusions: Pre-intervention, there were 101 one-time orders of IV labetalol and hydralazine, 70% of which were not indicated, as no evidence of hypertensive emergency and able to take PO. Of those orders, 39% lead to an adverse event, defined by a drop in blood pressure over 25% or a change in heart rate greater than 20 beats per minute. Moreover, 49% had documented alternate etiologies for blood pressure elevation, such as pain or agitation. Post-intervention, the number of non-indicated orders dropped from an average of 5.8 to 2.3 per week (60% reduction). Concurrently, the number of related adverse events dropped from an average of 8.2 to 2.6 per week (68% reduction). Our cost analysis estimated $55,093 annual cost to our hospital for these unnecessary IV medications. With our reduction in these orders, there is now a $32,850 reduction in cost. Our interdisciplinary implementation successfully demonstrated a reduction of unnecessary and harmful IV antihypertensives, which can be replicated in other institutions.