Background: Hospital Readmission Reduction Program(HRRP) implemented by CMS as part of Affordable Care Act (ACA) applies financial penalties to hospitals that have higher-than-expected readmission rates for common conditions such as AMI, pneumonia, and HF. CMS extended this program to include COPD for the fiscal year (FY) 2015. While there has been a reduction in readmissions, the impact of penalties on mortality in patients with COPD remains unknown. We aim to examine association of HRRP with mortality and readmissions in hospitalized patients with acute exacerbation of COPD(AECOPD)
Methods: We used Hospital Compare data on 30-day all-cause risk standardized mortality rate (RSMRs) and 30-day risk standardized-readmission rate (RSRRs) for COPD exacerbation from FY 2013-2017. We assessed the relationship between RSMRs and RSRRs using mixed linear models. Results were adjusted for African American percentage in hospital service area (HSA), HSA median income, ownership of hospital, teaching status, acute care hospital beds in HSA, percentage with insurance in HAS, and percentage of people living in poverty in HSA.
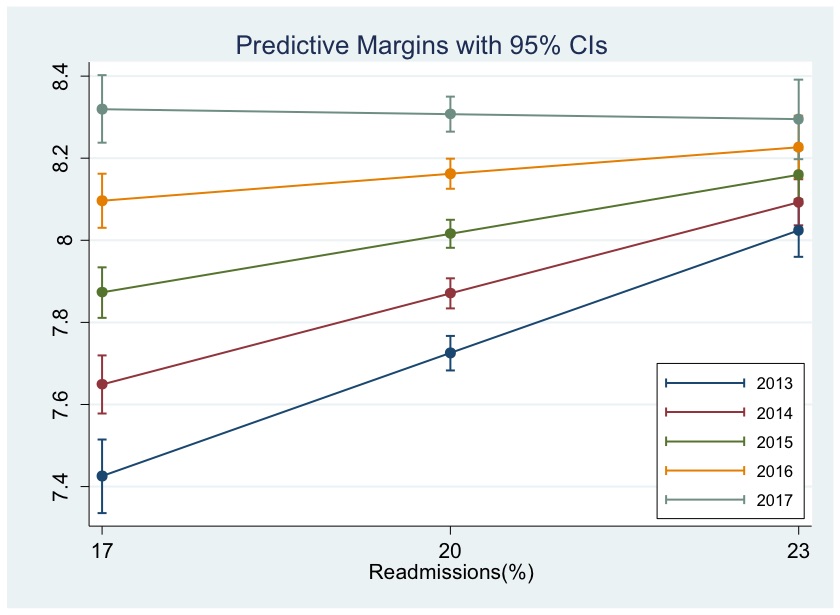
Results: Of the 3,685 acute care hospitals analyzed in 2013 data for COPD (pre-HRRP), the unadjusted mean 30-day all-cause risk standardized mortality rate (RSMRs) was 7.89%, this increased to 8.4% in 2017 (post- HRRP) at yearly rate of 0.13 (0.12 to 0.14; P<0.001) while mean 30-day risk standardized-readmission rate (RSRRs) declined from 20.7% to 19.6%. In mixed linear models, each 1% increase in RSRR was associated with a 0.10% (95%CI=0.08 to 0.12; P<0.001) increase in RSMR in 2013 but this relationship decreased by 0.027%/year (95%CI=-0.03 to -0.02; P<0.001) to statistically nonsignificant level in 2017 (-0.004%, 95%CI=-0.03 to 0.02; P=0.75) (Figure). When examined by the penalty status of hospitals in 2015, there was no difference in the rate of change in RSMR between hospitals that were penalized and those that were not (difference in rate of change/year = -0.001; P=0.99).
Conclusions: We found that while 30-day all-cause RSRR is decreasing, the RSMR is increasing from 2013 to 2017. We further found that while there does not appear to be a direct effect of penalties on the RSMR, there may be an indirect effect resulting in disappearance of RSMR-RSRR relationship across all hospitals. The underlying reason for this discordance may be related to HRRP but need to be explored further.