Case Presentation: A 32 year old female with morbid obesity presents with acute onset chest pain and dyspnea. Vitals notable for HR 130s, BP 117/71, RR 22, 99% RA. Cardiopulmonary exam was unremarkable. Labs were notable for troponin 0.266, BNP 679 and lactic acid 3.7. CXR was clear and lower extremity ultrasound was negative for DVT. CTPE demonstrated a large saddle PE with significant bilateral multi-level clot. She was found to have a large RV with septal flattening on TTE. The patient was started on heparin but became progressively tachycardic and tachypenic. She was taken urgently to the cath lab for catheter-directed thrombolysis (CDT). The patient’s clinical status improved during the remainder of her hospital course.
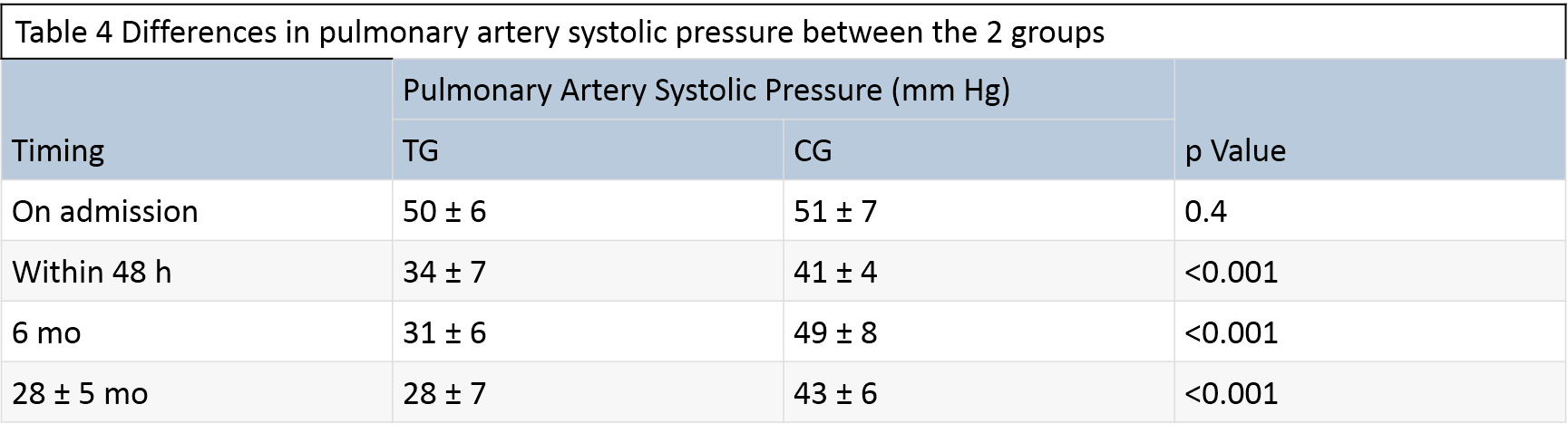
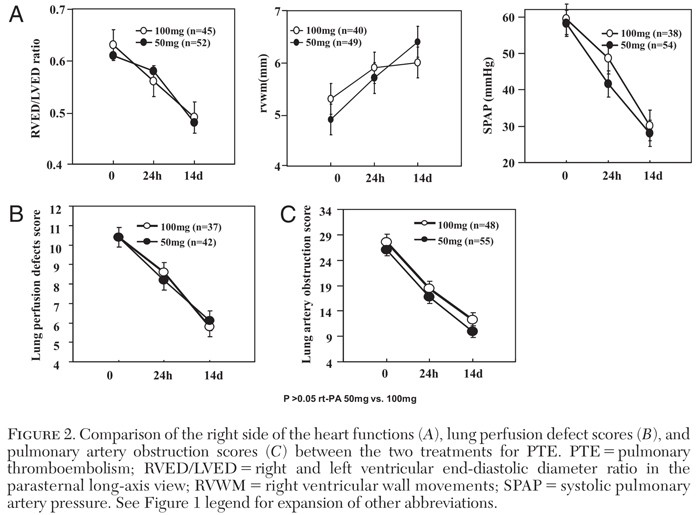
Discussion: An aggressive treatment approach should be considered for intermediate risk PE given the high associated mortality risk2. The use of tPA for intermediate risk PE is not recommended on a routine basis but may be considered for those with clinical evidence of adverse prognosis and low risk for bleeding complications1. Furthermore, the optimal dose, route of administration and duration of thrombolytic therapy remains unclear.In the MAPPET-3 Trial, systemic tPA was superior to heparin in preventing clinical deterioration requiring treatment escalation for intermediate risk PE driven primarily by an increased rate of rescue thrombolysis3. In the PEITHO Trial, there was reduction in hemodynamic decompensation at 7 days with systemic tPA (NNT 29). However, there was an increased risk for ICH and major bleeding with tPA (NNH 20)4. The unfavorable risk/benefit profile of thrombolytic therapy prompted the study of low-dose tPA. Compared to heparin alone, low-dose systemic tPA was associated with a significant reduction in the rate of pHTN within 48hrs and long term at 2.3 years without increased risk of major bleeding5. Similar improvements in RV function were noted at 24hrs and 14 days between low and full dose tPA with less bleeding risk associated with low dose tPA6. Studies evaluating CDT have shed more light on the dose-response curve for tPA. CDT allows for local delivery of tPA through a PA catheter amounting to a total dose that is a fraction of systemic tPA dosing. In the ULTIMA Trial, CDT significantly reduced RV dilation and improved RV function at 24 hours compared to heparin alone for intermediate risk PE with no major differences in bleeding rates7. The OPTALYSE PE Trial further evaluated lower doses of tPA and shorter infusion durations. A significant reduction in RV dilation without increased bleeding risk with doses as low as 4mg of alteplase administered through catheter over 2 hours was noted8. These results suggest that lower doses of systemic tPA may be as effective as the current standard dosing with less major bleeding complications. A comparison of systemic low dose tPA to CDT is ongoing9. The discordance in regards to the thrombolytic agent used, protocol for concomitant anticoagulation, as well as inclusion criteria and definition of intermediate risk PE limits the generalizability of the findings across these studies.
Conclusions: Thrombolytic therapy is not routinely recommended for intermediate risk pulmonary embolism but may be considered for high risk phenotypes. Thrombolytic therapy acutely decrease clot burden and improves RV function preventing clinical deterioration. Low dose tPA has been shown to improve RV function with lower bleeding risk. Determining the optimal dose of tPA, duration and route of administration should be the goal of future studies