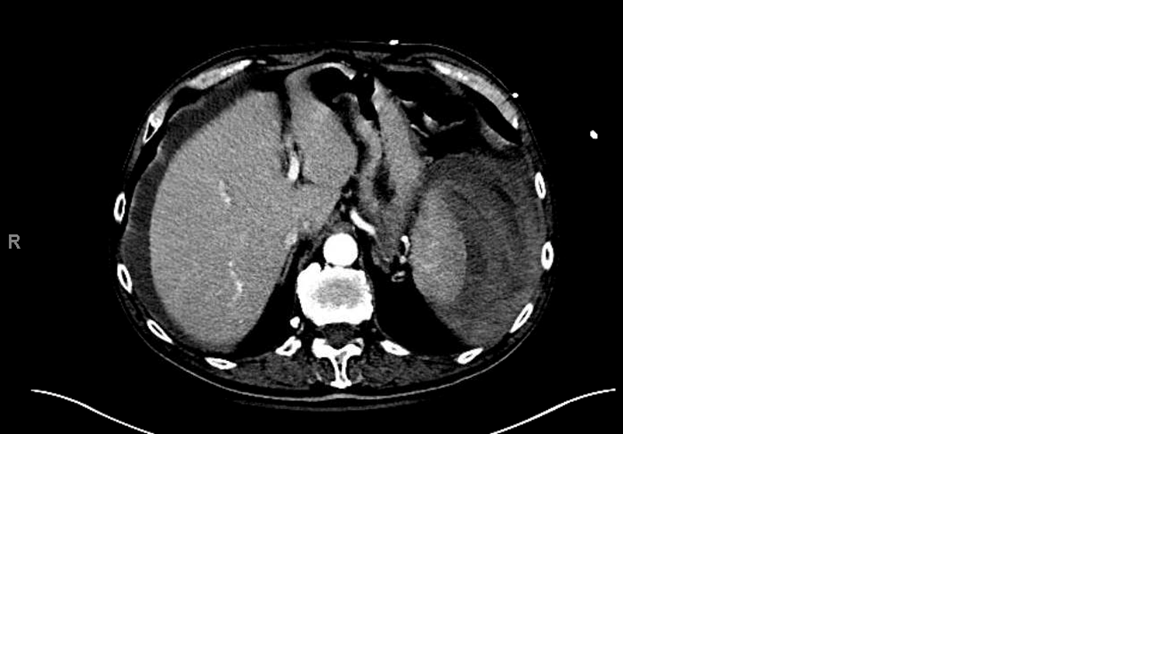
Case Presentation: An 86-year-old man with a history of atrial fibrillation on apixaban and aspirin for coronary artery disease presented with orthostatic syncope leading to a fall. Patient had complained of left upper quadrant abdominal pain the night prior to the fall. Patient denied trauma prior to the onset of abdominal pain, recent sore throat, fever, chills, night sweats, weight loss, fatigue, reflux, or recent travel. On presentation, blood pressure was 107/67 mm Hg and heart rate 65/minute. Physical examination was significant for diffuse bilateral abdominal tenderness without any guarding or rebound tenderness. Hemoglobin was 11.8 g/dl, down from a baseline of 14 g/dl. Coagulation panel revealed INR 1.2 (normal: 0.9-1.1), PT 14.9 seconds (normal: 11.7-14.1 seconds), PTT 28 seconds (normal: 23-34 seconds) and platelets 146,000/uL (normal: 130,000-400,000/uL). CT abdomen/pelvis with contrast showed active extravasation from the spleen with a large subcapsular hematoma with hemoperitoneum. He was treated with prothrombin complex concentrate, 2 units packed red cells, and splenic artery embolization. Despite this, several hours later the patient became acutely hypotensive. Ultrasound at bedside showed large hemoperitoneum. Patient underwent urgent exploratory laparotomy with splenectomy. Splenic pathology revealed capsular disruption with associated sub-capsular and intra-parenchymal hemorrhage, and numerous macrophages within the splenic parenchyma likely secondary to a reactive phenomenon. The patient had a good recovery and his apixaban was resumed upon discharge.
Discussion: Atraumatic splenic rupture is a rare but life-threatening condition with mortality as high as 12%. Although splenic pathology is frequently associated with rupture, it can rarely occur in completely normal spleens, and can be more serious if patient is anticoagulated. Atraumatic splenic rupture has been reported in patients on anticoagulants, and can be life-threatening. Any occult splenic pathology may predispose to bleeding. Physicians caring for patients on anticoagulation with unexplained shock should consider atraumatic splenic rupture as a cause, and intervene quickly.
Conclusions: Atraumatic splenic rupture can occur in patients on anticoagulants with disastrous consequences. In these patients, physicians should consider atraumatic splenic rupture as a cause of unexplained shock, and intervene quickly.