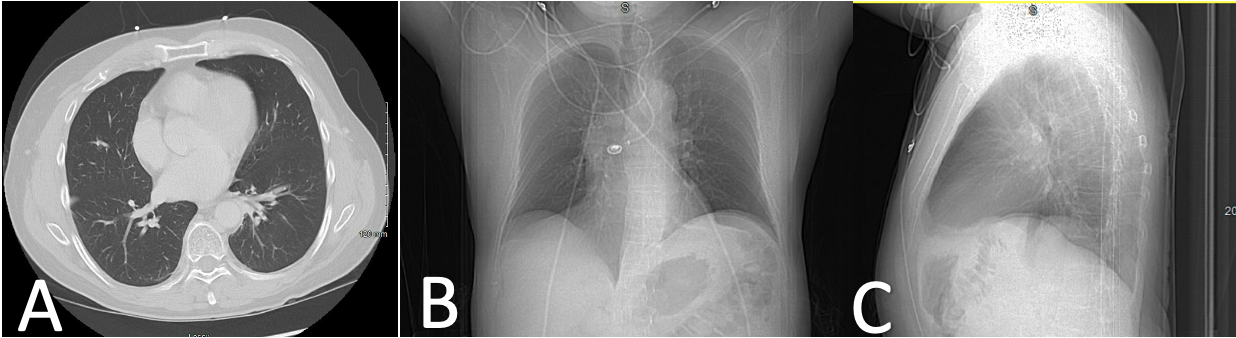
Case Presentation: A 43-year-old male with a history of diffuse large B-cell lymphoma (DLBCL) in remission for 2 years after chimeric antigen receptor (CAR) T-cell therapy presented to his PCP with headaches and a mild cough. A PCR COVID-19 test was positive, a head CT showed cerebral edema, and MRI had diffuse dural thickening without signs of malignancy. NSAIDs were recommended. Three weeks later, he presented to the ED with progressively worsening headaches and mild dyspnea; repeat MRI showed resolution of dura thickening, and lumbar puncture was negative for lymphoma or infection. He was discharged on antibiotics for community-acquired pneumonia with a residual dry cough. A month later, he presented to the ED with a productive cough and fever. CXR showed bilateral alveolar infiltrates, and follow-up chest CT showed bilateral ground glass opacities (Figure 1). Suspicious of multifocal healthcare-associated pneumonia, he was started on empiric antibiotics. Aside from another positive COVID-19 PCR test, his infectious workup was negative. Furthermore, he remained febrile despite treatment. Post-COVID-19 organizing pneumonia was suspected, and he was switched to corticosteroids (prednisone 40mg daily) with a 3-week taper, which improved his condition. Two weeks later, he presented to another ED with fever, tachycardia, dyspnea, and hypoxia. Chest X-ray showed recurring airspace infiltrates and decreased lung volumes (Figure 2). He was placed on supplemental oxygen, and started on broad-spectrum antibiotics. Aside from a positive COVID-19 PCR test, his infectious workup was again negative. A trans-bronchial biopsy showed hyaline membranization and severe epithelial atypia, consistent with severe lung injury. He was given high-dose methylprednisolone with a long-term oral taper. He was weaned off oxygen and improved in condition.
Discussion: Despite most COVID-19 infections being mild cases, patients with malignancy who get COVID-19 often have severe respiratory distress with high mortality rates.(1,2) To our knowledge, no case has previously described a prolonged, serum-positive COVID-19 pneumonitis causing severe lung injury with clinical improvement from a high-dose methylprednisolone taper. Golbets et al. (2021)(3) similarly describes a patient with a history of DLBCL, on maintenance rituximab, who clinically improved after introducing corticosteroids to treat secondary organizing pneumonitis in the setting of COVID-19 and no other infectious etiology. In contrast, corticosteroids were not used to treat prolonged COVID-19 pneumonitis in a patient with immunocompromised status on CAR-T therapy, who subsequently died from respiratory failure. (4) Corticosteroids may partly explain the differential outcomes in these patients. More research is needed to understand the role of corticosteroids in prolonged COVID-19 pneumonitis with pulmonary manifestations.
Conclusions: Due to the novel nature of long-COVID syndrome, no guidelines exist for the therapeutic management of patients with chronic, serum-positive COVID-19 pneumonitis and diffuse lung injury. This case suggests a need to be vigilant with COVID-19 in patients with a history of malignancy and immunosuppression. Perhaps early recognition and treatment with steroids might reduce the incidence of severe lung injury in this population.