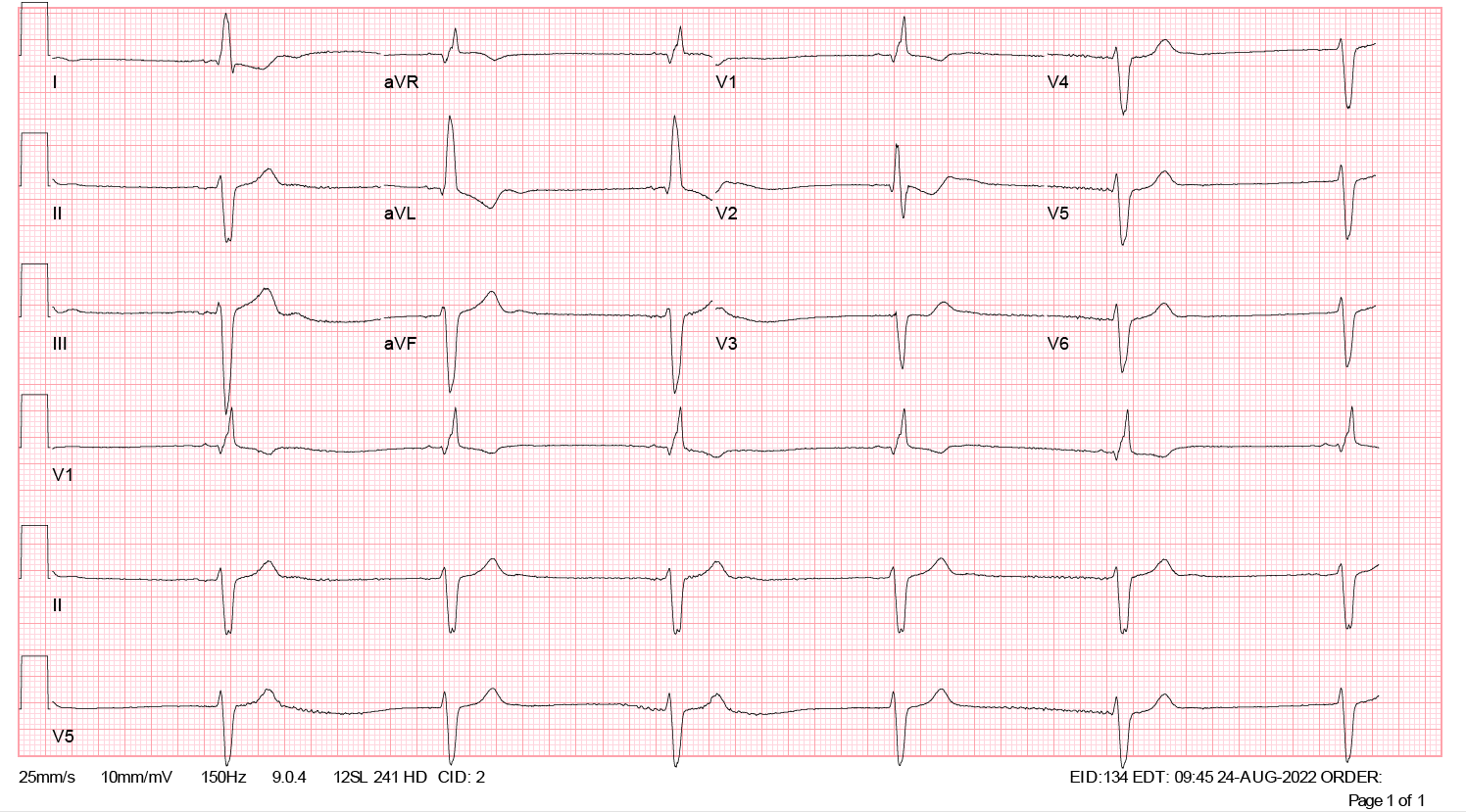
Case Presentation: An 83-year-old male with a history of paroxysmal atrial fibrillation, severe congestive heart failure, and end-stage renal disease on hemodialysis presented to the emergency department from outpatient dialysis for symptomatic bradycardia. He endorsed dizziness, dyspnea on exertion, and weakness. Additional history revealed he was recently admitted for a heart failure exacerbation and instructed to discontinue digoxin at discharge. However, he had continued to take the medication outpatient. At presentation, he was hemodynamically stable on room air but bradycardic (BP 134/70, HR 37). Exam showed JVP at the nape of the neck without significant peripheral edema. Baseline labs and thyroid function testing were relatively unremarkable, except for a potassium level at the upper limit of normal of 5.1 mEq/L. Serum digoxin level was found to be markedly elevated at 4.7 ng/ml. ECG was notable for an idioventricular rhythm and bradycardia with rates in the 30s, consistent with digoxin toxicity. He was subsequently admitted to the cardiac critical care unit for close monitoring, and nephrology was consulted. His home metoprolol succinate and amiodarone were held. He received 4 vials of digoxin-specific antibody antigen-binding fragments (DSFab), underwent hemodialysis for 5 hours, and was placed on continuous renal replacement therapy for an additional 48 hours. A repeat serum digoxin level was drawn and found to be 7.2 ng/ml; no further levels were drawn. At discharge, his bradycardia had completely resolved. He was given clear verbal and written instructions to discontinue digoxin and restart his home metoprolol.
Discussion: Digoxin toxicity is a clinical diagnosis, but elevated levels at presentation can aid in prompt diagnosis and treatment. First-line therapy is DSFab, and serum digoxin levels should not be measured after administration due to nonspecific binding of test reagents with DSFab leading to falsely elevated levels, as demonstrated in this case. Additionally, patients with end-stage renal disease are at increased risk of rebound toxicity due to dissociation of the DSFab-digoxin complex and should be monitored closely after administration. Although this patient received hemodialysis, dialysis is not a first-line treatment for digoxin toxicity because of the drug’s high volume of distribution. However, it is indicated if the patient has concomitant renal failure and/or electrolyte derangements.
Conclusions: Digoxin is a cardiac glycoside that is used in patients with congestive heart failure and/or atrial fibrillation due to its positive inotropic and negative chronotropic effects. However, it has a narrow therapeutic index and should be monitored closely in patients with renal failure. Serum levels should be interpreted with caution in the context of a patient’s treatment course.