Background: Medication reconciliation at patient care transition points is a requirement of multiple regulatory bodies in medicine. In 2005 it was rated as the #8 National Patient Safety Goal by the Joint Commission and subsequently as the #3 goal in 2011. The Center for Medicare and Medicaid made medication reconciliation part of its Meaningful Use project and stated that in May of 2014 greater than 50% of patients admitted to the hospital should have this completed within 24 hours of admission. Despite the implementation of electronic medical records and electronic medicine reconciliation tools, institutions still have opportunities to improve on this important initiative to avoid adverse drug events.
Purpose: After a change to our electronic health record, there was a noticeable decrease in compliance with admission medication reconciliation. We aimed to improve our rate of medication reconciliation upon admission to our institution by generating a personalized automatic email to any provider who did not perform a medication reconciliation upon admitting a patient to the hospital. The data presented here is abstracted from our larger project and is specific to the internal medicine resident teaching service.
Description: We generated a report through a Structured Query Language (SQL), a programming language that allows for custom reports of a specific subset of data from a large database such as one used to store electronic health records. This report generated a list of patients who were currently admitted to the hospital but had incomplete medication reconciliation, along with the name of the provider who had put the admission orders in the electronic health record. We then wrote a macro in visual basic that was executed in Microsoft Excel that automatically generated an email to the admitting resident reminding them upon admission, a medication reconciliation needed to be performed. Based on resident feedback, we realized many residents were performing the medication reconciliation but not clicking on a specific button that stated it was done and finalized the process. This button was a new addition to our electronic medical record in July 2014. We then performed a second intervention by modifying our email to remind them to click the button. After receiving feedback that indicated the providers did not know where the button was, we performed a third intervention and modified our email again to add a screenshot of the location of the button.
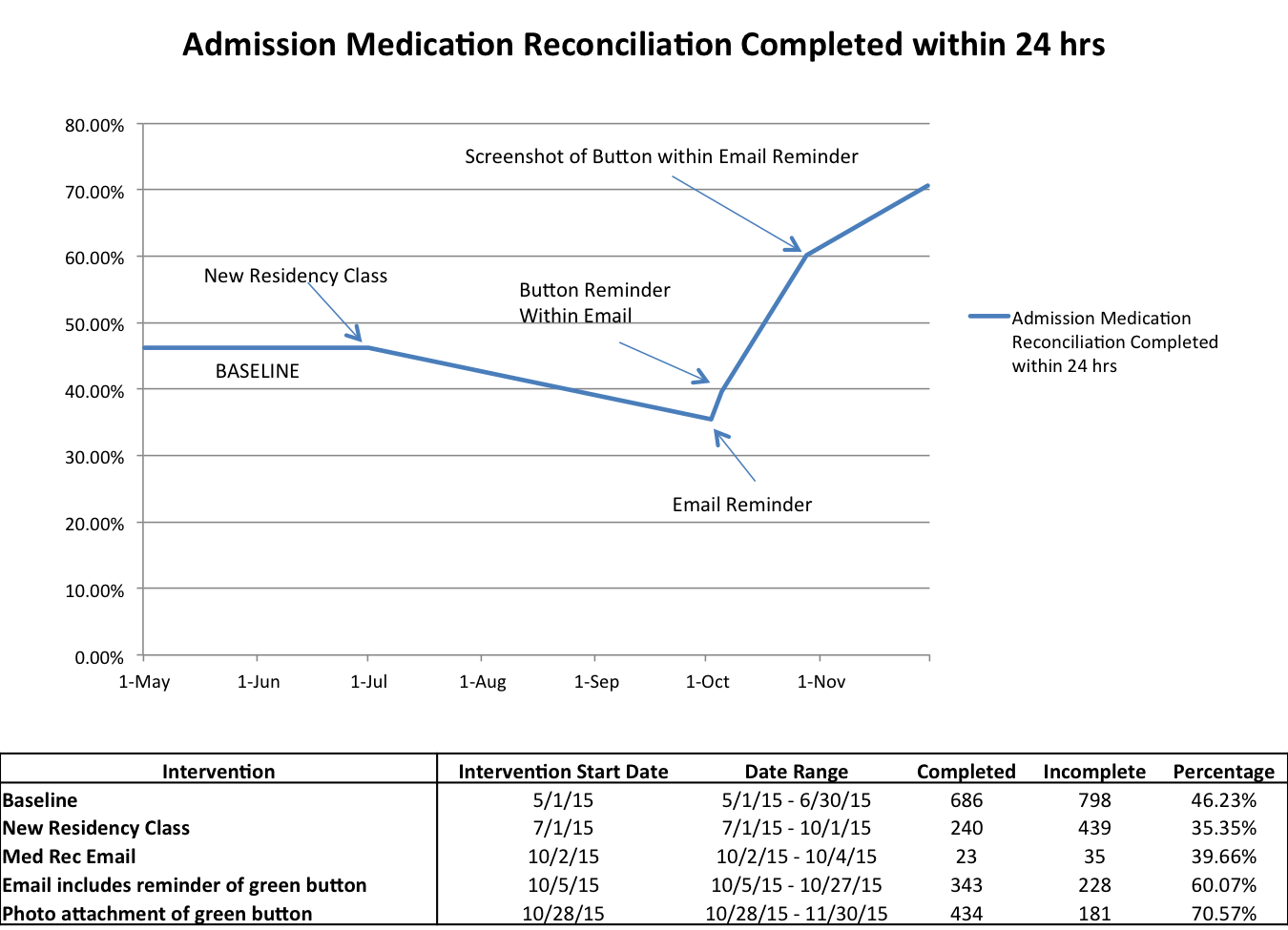
Our baseline admission medication reconciliation completion compliance rate from May to June of 2015 was 46.23%. The compliance rate declined to 35.44% after the introduction of a new residency class on July 1st. After sending email reminders (Intervention #1), compliance increased to 39.66%. After adding the reminder to click the button (Intervention #2), compliance increased to 60.07%. After adding a screenshot to the email (Intervention #3), compliance increased to 70.57%
Conclusions: Using automatic, personalized, and targeted electronic reminder emails that included educational tips on how to complete the medication reconciliation has been an effective tool to increase our compliance rate and meet the standards set by CMS.