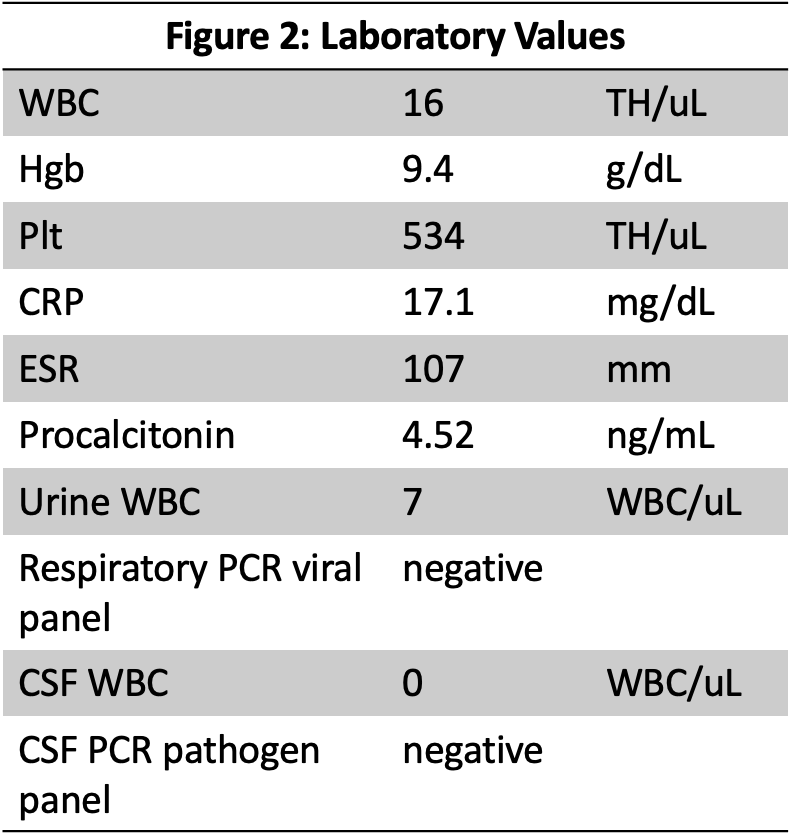
Case Presentation: A 57-day old ex-term, Caucasian female presented with one day of diffuse rash and fever in the setting of congestion and a sick sibling. Her rash was initially attributed to viral erythema multiforme. She was well-appearing but given vulnerable age and elevated band count, she was admitted for observation. With improvement of her rash and fever, and blood culture negative at 24 hours, she was discharged. However, she presented the next day with recurrence of fever and rash. Physical exam showed increased irritability, fever to 103.7F, and an erythematous, slightly raised, blanching, migratory, and coalescing rash with several targetoid lesions (Figure 1). She had mild swelling of the hands and feet. There was no lethargy, meningismus, conjunctival injection, oropharyngeal erythema or lesions, or cervical lymphadenopathy. Laboratory evaluation revealed marked inflammation, and infectious studies were negative (Figure 2). The persistent fever, rash, and systemic inflammation was concerning for Kawasaki disease (KD). An echocardiogram revealed Z scores of 1.9 and 1.2 for the right and left anterior descending coronary arteries, respectively, so intravenous immunoglobulin and aspirin were initiated on day four of illness resulting in marked clinical improvement, with resolution of fevers and down-trending inflammatory markers.
Discussion: KD is an acute vasculitis and the most common cause of acquired heart disease in children. The peak age of incidence in the U.S. is 2 years old; however, the disease can be seen even before the second month. It has historically been diagnosed by fever lasting at least 5 days in addition to clinical features of inflammation (conjunctival injection, polymorphous exanthem, cervical lymphadenopathy, distal extremity swelling with red palms and soles, and oropharyngeal erythema). Clinical presentation in young infants may be more subtle or incomplete, though laboratory values of inflammation are similar to older children. In addition, a single county study showed a significant proportion of clinicians, especially primary care physicians, did not consider KD in their differential diagnosis of children younger than 6 months. Furthermore, infants are at higher risk of morbidity and mortality even if appropriately treated within the first 10 days after fever onset. Infants may develop coronary artery dilation or aneurysm even before 5 days of fever. Therefore, more favorable outcomes result when diagnosis and treatment are initiated early.
Conclusions: Not only is the diagnosis of KD in infants less than 6 months old more difficult than in older children, but this population is also at higher risk of early coronary artery damage. Early diagnosis and treatment by primary care physicians and pediatric hospitalists is critical for favorable outcomes. The illness can easily mimic viral exanthems as was seen in this case. This infant benefited from suspicious clinicians, strict return precautions, diligent parents, and proximity to a quaternary children’s hospital. All clinicians must have a high index of suspicion for KD in young infants with only rash, fever, and non-specific inflammation on laboratory analysis. The American Heart Association guidelines urge obtaining an echocardiogram for such patients.