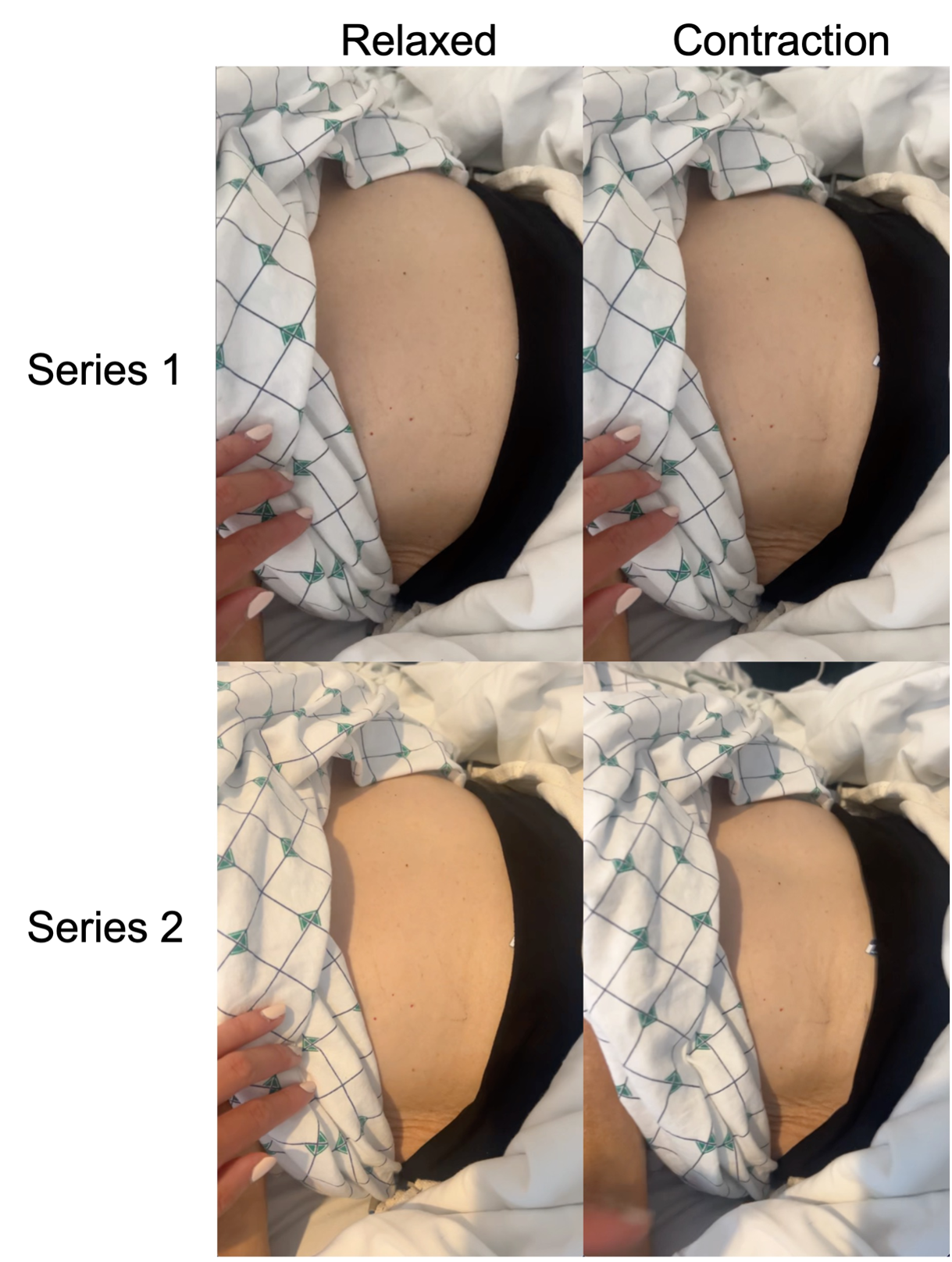
Case Presentation: A 70-year-old woman with hypereosinophilic syndrome (HES) complicated by recurrent organizing pneumonia (OP) was admitted to a hospital medicine service with four weeks of involuntary spasms of her abdominal wall muscles and hypoxemia. She reported having similar episodes during past OP flares which resolved quickly with prednisone. Notable admission vitals included a heart rate of 112 bpm and oxygen saturation of 82% on room air that normalized with 2-3 L of supplemental oxygen. On exam, the patient had episodic abdominal spasms lasting from twenty minutes up to several hours. The movements localized to the abdominal wall and were characterized by rapid, repetitive, and involuntary contractile spasms (Figure 1). The spastic movements occurred only in the abdomen and did not radiate. During episodes, patient developed increased work of breathing and desaturations requiring 4-6 L of supplemental oxygen. Neurology and pulmonary were consulted. MRI brain and spine did not reveal suspicious structural lesions. CT chest showed basal and peripheral predominant, peribronchovascular/perilobular ground-glass consolidation and septal thickening consistent with an OP flare, for which she was started on prednisone 60mg daily. With unrevealing work up and further literature review, she was diagnosed with presumed abdominal segmental myoclonus (ASM), also known as “Belly dancer’s dyskinesia”. Given the severity of her symptoms and worsening hypoxia during these episodes, she was started empirically on baclofen and flexeril, which were ineffective and discontinued. Clonazepam 0.25mg twice daily was started and produced significant clinical improvement with reduced frequency and severity of abdominal spasms. Clonazepam was subsequently increased to 0.5mg twice daily. Over a nine-day hospitalization, the patient’s abdominal spasms decreased substantially in frequency and severity, and her hypoxia also gradually resolved.
Discussion: ASM is a very rare disorder largely described in case reports and characterized by focal dyskinesia of abdominal wall musculature causing writhing movements. ASM should be included in the clinical differential for abdominal spasms and is associated with various etiologies including central and peripheral neurologic lesions of structural, autoimmune, osmotic demyelinating, and drug-induced origins 1, 2.Although similar presentations of ASM have been observed in patients with upper respiratory infections including SARS-COV2 3, this is the first report of ASM in a patient with HES and recurrent OP. Acute hypoxia is an additional, uncommon complication.This patient’s ASM preceded symptoms of an OP flare. Her hypoxemic respiratory failure was likely due to both the underlying OP flare and impaired chest wall mechanics due to ASM, as her hypoxia was observed to worsen during episodes of ASM.Guided by the limited literature, she was treated with clonazepam for symptom control. The patient’s symptoms of ASM improved substantially with both treatment of underlying OP flare and low-dose clonazepam.
Conclusions: Hospitalists frequently care for patients with interstitial lung disease flares, and this is the first known case of ASM in a patient with OP including with ASM as a presenting complaint for an OP flare. Additionally, this adds further support for the use of clonazepam as an effective therapy for symptomatic control in these patients.