Background: The Discharge Summary (DS) plays a vital role in transmitting key information about a patient’s hospital admission to their primary care clinician (PCC) and serves as a valuable information source for inpatient clinicians. However, current guidelines for DS creation tend to neglect the importance of prioritizing critical content. This oversight, coupled with the excessive auto-population of data into DS templates by Electronic Health Records (EHRs), has resulted in “note bloat,” making DSs lengthy, challenging to read, and less effective in communicating essential patient information. Previous research has shed light on the patient safety risks associated with these DSs, underscoring the importance of equipping clinicians and learners with the skills to compose high-quality DSs. Clinicians typically allocate only 1-5 minutes to review DSs, thus brevity should be prioritized. To improve and standardize the DS, we initiated a two-phase project. In Phase 1, we conducted a comprehensive survey involving only outpatient clinicians across multiple sites and disciplines. Subsequently, in Phase II, we present the findings from a survey focused on inpatient clinicians’ DS uses and preferences with the goal of optimizing documentation for the seamless transition of care between all healthcare settings.
Methods: From January to June 2022, in Phase II, we carried out a national survey distributed to 1723 clinicians that garnered a 31% response rate. This geographically diverse, multisite (including 6 hospital systems), multidisciplinary survey focused on inpatient clinicians across various levels of training to examine their usage patterns and preferences regarding DSs. The inpatient clinicians included in Phase II were hospitalists, intensivists, internal medicine residents, critical care fellows, emergency room doctors, pediatric hospitalists, and acute care advanced practice providers. The surveys were administered through Qualtrics electronically as well as some distributed in person.
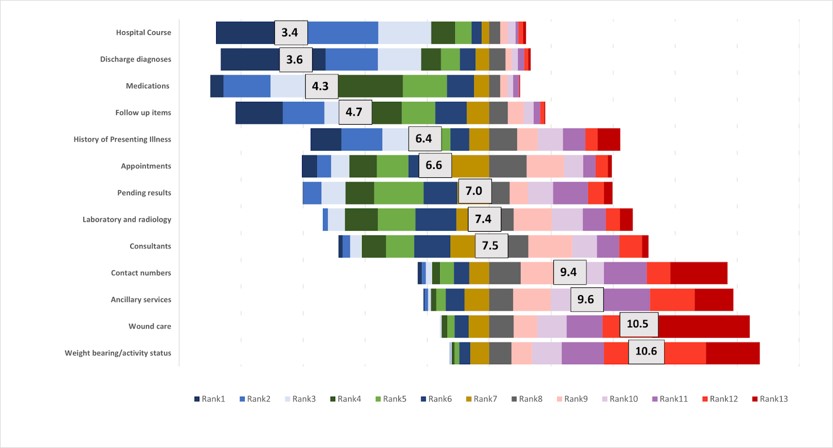
Results: The Phase II analysis, consistent with our Phase 1 findings, demonstrated significant consensus in prioritizing components across both institutions as well as clinician types (inpatient vs. outpatient). Remarkably, as shown in Figure 1, the top 4 and bottom 4 DS components remained consistent across all institutions and clinician types. The top 4 components were Hospital Course, Discharge Diagnoses, Medication Reconciliation, and Follow-up, while the lowest ranked components were Contact Numbers, Ancillary Services, Wound Care, and Activity Status. While we identified minor yet statistically significant differences in preferences linked to the level of training, a consensus persisted among specialties within a given training level and between institutions, even those employing different EHRs.
Conclusions: These findings provide strong support for the implementation of a standardized DS template, highlighting a striking consensus among clinicians, irrespective of where in the United States they practice, or their roles as inpatient or outpatient clinicians. This further emphasizes the importance and practicality of adopting a universal standardized DS template to improve DS quality and patient care by facilitating efficient and standardized communication across various healthcare settings.