Background: Interest in quality improvement (QI) has increased exponentially in recent years throughout medicine. However, most QI educational resources have been centered at university-based hospitals. Less well-resourced community hospitals may have less access to these QI resources and encounter substantial challenges including an unwelcome culture towards QI, difficulty engaging stakeholders, and interpersonal conflicts. Due to these challenges, developing QI skills alongside leadership, team management, and organizational change skills may further enhance success of QI projects, particularly at community hospitals affiliated with a university-based hospital.
Purpose: 1. Describe a novel program aimed at helping physicians build both QI and leadership skills to develop QI projects within regional community hospitals. 2. Explore program participants’ perceived skill acquisition prior to and after completion of the program, and participants’ evaluation of the program.
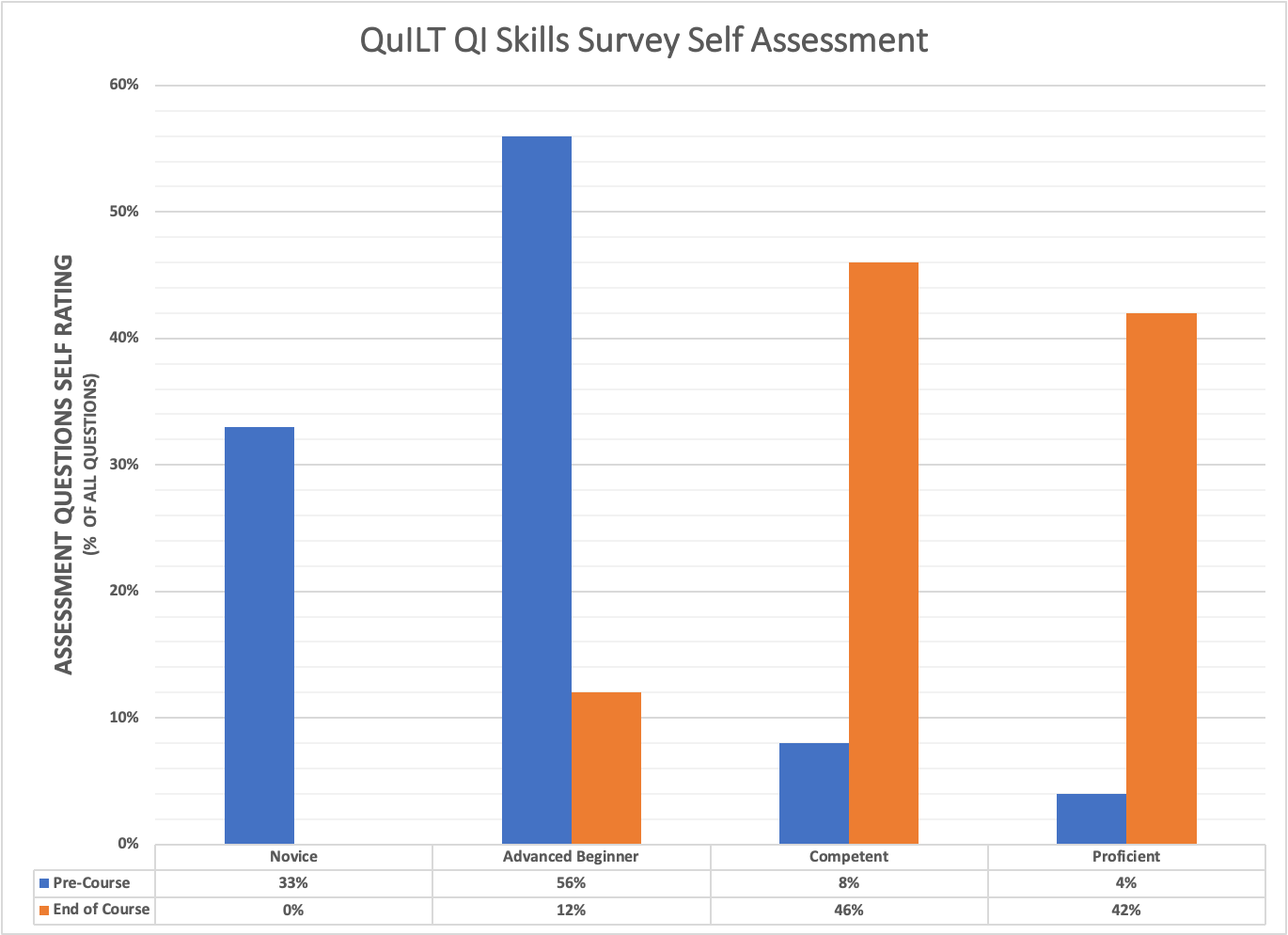
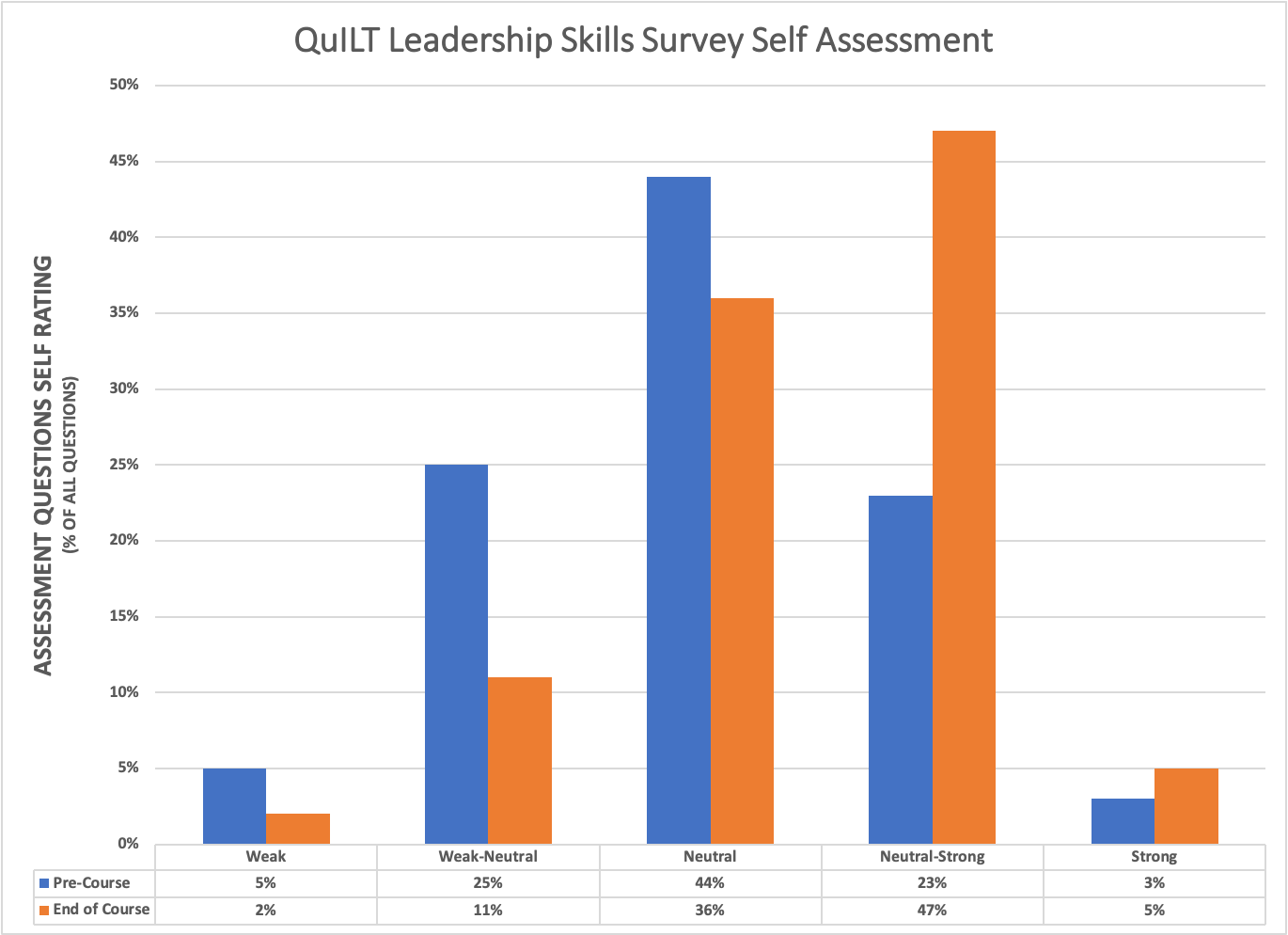
Description: A 9-month longitudinal Quality Improvement and Leadership Training (QuILT) program was developed for physicians within a regional network of community hospitals affiliated with a university-based center. The program consisted of monthly educational sessions by local and national speakers in both QI and Leadership topics, as well as required reading in QI and Leadership, a personal leadership skills assessment survey, and individual coaching for participants. Metrics used to evaluate the impact of the program included a Leadership Skills Assessment Survey and an original survey assessing an individual’s comfort with QI skills and leadership skills administered both at the initiation and completion of the program. Four physicians were selected from 7 applicants to participate in QuILT. All participants were from affiliated community hospital site programs; two of which were from the same community hospital site, while the others were from two separate community hospitals. Of the 4 participants, 3 were 0-3 years out of residency, while 1 was 8-11 years beyond residency training. Only one of the 4 cohort members had previous formal training in QI. Prior to the program, 33% of participants perceived themselves as having “Novice” and 56% having “Advanced Beginner” understanding and comfort in most QI skills. Similarly, 25% of participants rated themselves as having “Weak-Neutral”, 44% having “Neutral”, and 23% having “Neutral-Strong” understanding and comfort in most Leadership skills at the initiation of the program. At the end of the program, 46% stated as having “Competent” and 42% stated as having “Proficient” understanding and comfort in most QI skills. Leadership skills assessment at the end of the program demonstrated 36% having “Neutral” and 47% having “Neutral-Strong” understanding and comfort in most skills. All participants also reported feeling “satisfied” or “very satisfied” with their overall educational experience in the program.
Conclusions: A structured and individualized combined QI and Leadership training program for physicians working within community hospitals is a novel approach that can increase understanding and comfort in developing QI projects. This can also expand the effects of QI initiatives that are centered at the main university-based center to the surrounding region. Future studies should investigate the relative effectiveness between this hybrid QI-leadership model compared to traditional QI education.