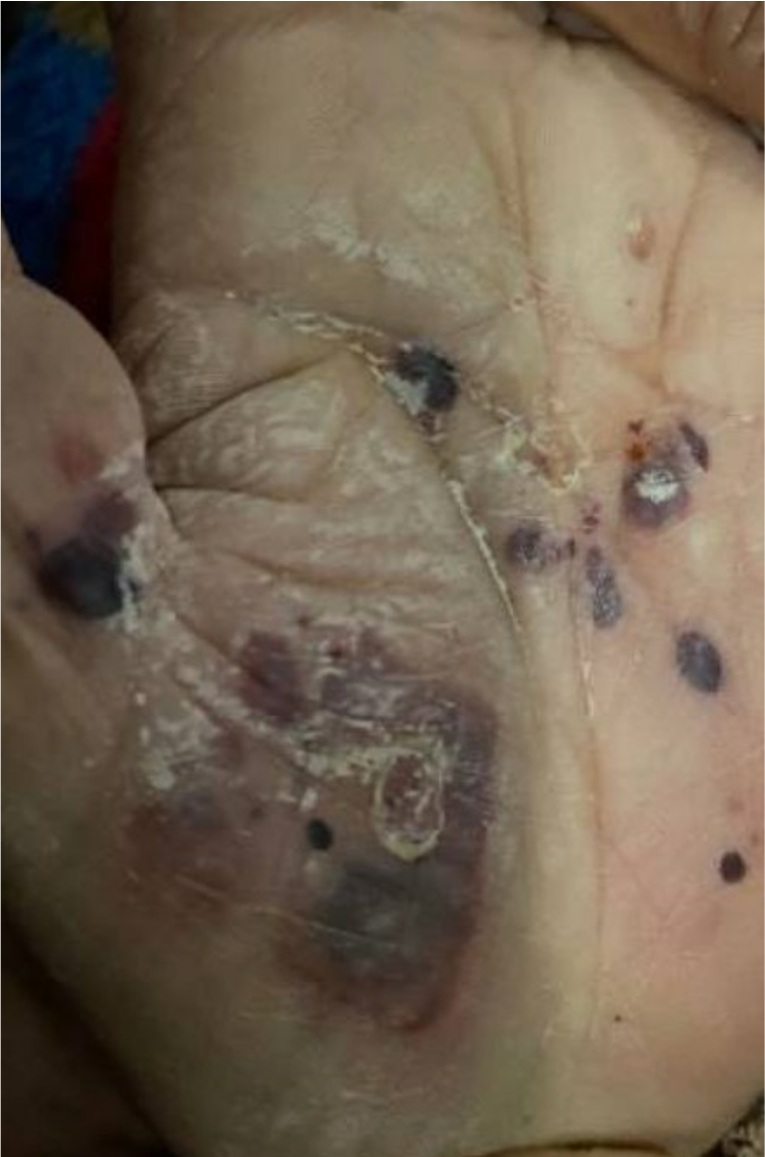
Case Presentation: An 80-year old woman with a PMH of a hemorrhagic R thalamic CVA, CKD3, HTN, HLD, T2DM presents for weakness and fevers in the setting of a 1 month long diffuse rash. The rash began on her legs, but spread to gluteal region, chest, arms, and palms/soles. The lesions started as blisters that ruptured, eroded, and healed without scarring. An outpatient dermatologist that stopped several diabetes medications including linagliptin and dulaglutide. After that visit, the patient became more lethargic and began to have fevers. After admission, the patient was treated for secondary infection. Two lesions were biopsied. Histology was notable for spongiotic dermatitis with rare eosinophils in the epidermis, superficial perivascular lymphohistiocytic infiltrate with frequent perivascular, and interstitial eosinophils in dermis pointing towards urticarial phase of BP. Direct immunofluorescence was notable for linear IgG and C3 deposits at the dermal-epidermal junction. BP180 IgG Ab was 142 U/mL (nml < 9) and BP230 IgG Ab was 21 (nml < 9). The patient began on prednisone 40mg daily, doxycycline 100mg twice daily. Niacinamide 500mg twice daily was initiated on discharge. Throughout hospitalization, the patient did not develop any new blisters. At her initial follow-up, the patient was started on a prednisone taper, however a new lesion appeared. Additionally, the patient developed esophagitis due to doxycycline. Her regimen was adjusted to prednisone 10mg daily, dapsone 25mg daily, niacinamide, and topical bethamethasone 0.05% daily (for the new lesion).
Discussion: First described in 1953 by Dr. Walter Lever, bullous pemphigoid (BP) is now considered the most common autoimmune blistering diseases [1, 2]. Usually affecting elderly individuals, the incidence is increasing worldwide [1, 2]. BP occurs when a trigger initiates an auto-antibody mediated process leading to a destructive inflammatory cascade against the epithelial basement membrane. Two main antigenic targets have been identified, BP180 and BP230, both components of the hemidesmosome [1]. Titers of anti-BP180 correspond with disease activity [1]. BP presents with pruritic, tense blisters (serous or hemorrhagic) on an erythematous/edematous base on trunk or extremities with variable involvement of the mucosa that heal without scarring [1, 3]. Medications are known triggers and include dipeptidyl peptidate 4 inhibitors (DPP-4i), TNF-alpha inhibitors (adalimumab, etanercept, infliximab), antibiotics, and immune checkpoint inhibitors (pembrolizumab, nivolumab) are among the many implicated [2, 4]. Other triggers include vaccinations, infections, transplantation, and physical factors such as trauma, surgery, burns, UV exposure, and radiotherapy [4]. Treatment options include high-dose topical steroids, systemic steroids, doxycycline, dapsone, azathioprine, mycophenolate mofetil, methotrexate, rituximab, dupilumab, omalizumab, and IVIG [1, 5]. First line therapy includes topical or systemic steroids +/- doxycycline and niacinamide supplementation. The exact trigger for our patient is unclear as the patient was started both on a DPP-4i and GLP-1a, which has been associated with BP in a few case reports.
Conclusions: BP should be on the differential for the presentation of any blistering skin rash. A full medication review is necessary as prompt discontinuation of offending agents is imperative. Morbidity and morality rates can be high, so it is important to treat quickly with a combination of steroid and non-steroidal agents.