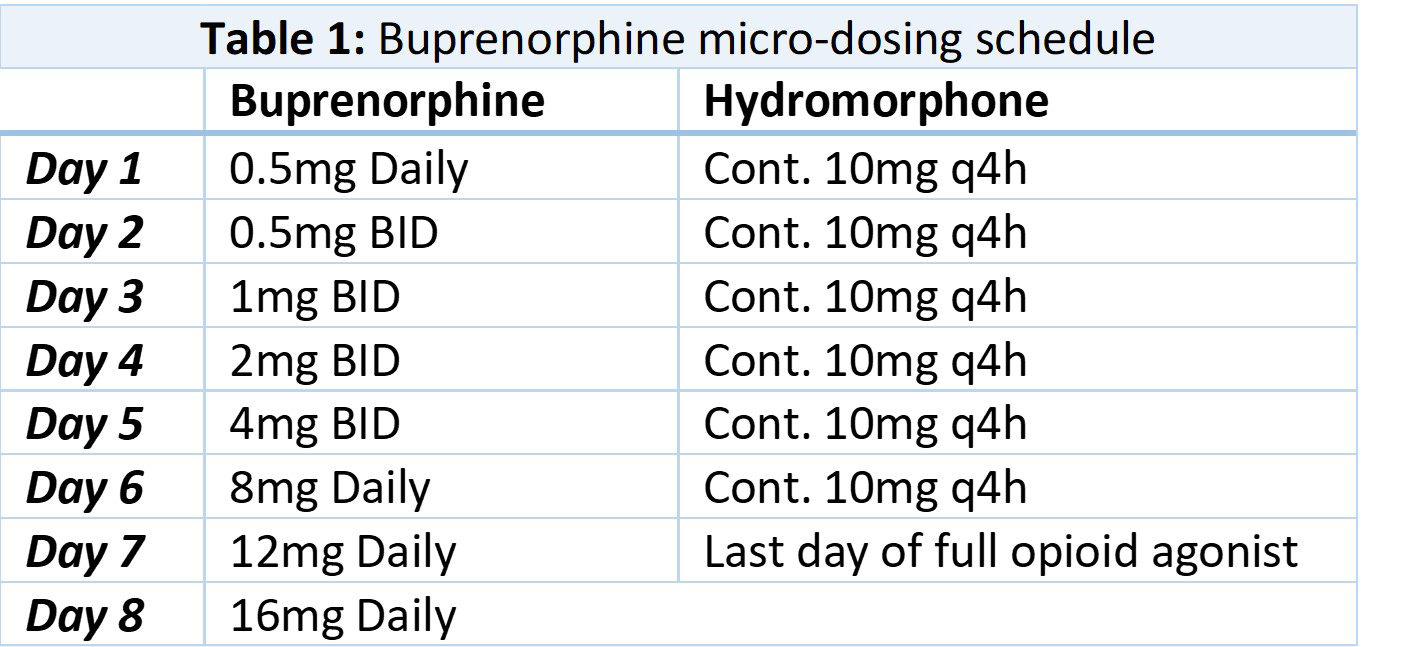
Case Presentation: A 37-year old woman with a past medical history of opioid use disorder (OUD) and hepatitis C was admitted to a tertiary care center for management of septic shock from necrotizing soft tissue infection secondary to injection drug use, requiring multiple operations with subsequent skin grafting. She reported using multiple grams of intravenous heroin daily prior to admission, thereby requiring high doses of full opioid agonists to achieve adequate post-operative pain control due to her high opioid tolerance. The patient desired starting buprenorphine for OUD but was concerned about experiencing withdrawal and increased pain. With the patient’s consent, Buprenorphine micro-dosing was initiated to transition from hydromorphone to avoid precipitating withdrawal and still maintain effective analgesia. While continuing hydromorphone 10mg oral q4h, small doses of buprenorphine were administered daily to slowly displace the full mu agonist from opioid receptors over a 7 day period. The regimen started with sublingual buprenorphine 0.5mg on day one, then 0.5mg BID on day two, and continued up-titration to 16mg on day 8 [table 1]. Hydromorphone was discontinued on day 8 without taper as the full agonist had been displaced by the highly receptor-avid buprenorphine. Throughout the induction period she denied any withdrawal symptoms. The patient was discharged on buprenorphine instead of a full mu agonist. Her pain was well controlled, and her OUD was in early remission.
Discussion: Buprenorphine is a partial mu receptor agonist indicated for the treatment of OUD. Buprenorphine decreases mortality in OUD as well as treating pain, withdrawal, and cravings. Its pharmacokinetic properties of high receptor binding affinity and slow dissociation from the mu opioid receptor can cause precipitated withdrawal in patients who are opioid dependent and whose receptors are saturated with full agonists. Patients usually need to wait 8-12 hours after the last dose of short-acting full agonists before buprenorphine initiation to avoid precipitated withdrawal. This phase is frequently difficult for hospitalized patients to tolerate due to uncontrolled pain during the acute period following an injury or surgery. Titrating up the partial mu agonist slowly displaces the full agonists from the receptors without inducing physiologic withdrawal. While increasing the partial mu agonist, receptor saturation and pain control in patients with an OUD can be safely achieved even with continuation of full opioid agonists. Initiating sublingual buprenorphine micro-dosing inpatient addresses OUD and acute pain while concurrently treating the primary reason for admission. A sublingual buprenorphine micro-dosing strategy facilitates initiation for medications for opioid use disorder (MOUD) in an evidence-based approach while effectively managing pain and withdrawal in the inpatient setting.
Conclusions: This patient’s case highlights a novel approach to the initiation of sublingual Buprenorphine in a stepwise fashion in admitted patients with OUD suffering from acute pain. Initiation of buprenorphine while inpatient instead of discharging on a full agonist is protective from an opioid overdose and increases likelihood of outpatient follow up for continuation of MOUD. Buprenorphine micro-dosing is an effective way for hospitalists to manage a patient’s OUD while also treating acute pain.