Background:
Readmissions cause significant distress to patients and caregivers in addition to considerable financial costs. A key component of reducing readmissions is identification of at‐risk patients prior to discharge. This determination currently is commonplace, as providers make informal predictions of readmission during routine care. However, the accuracy of these informal predictions, or more formal algorithm‐based approaches, are unknown. The goal of this study was to evaluate how well physicians, case managers, and nurses can predict whether their patients ≥ 65 years old will be readmitted and to compare their predictions to a standardized risk tool (probability of repeat admissions, or Pra).
Methods:
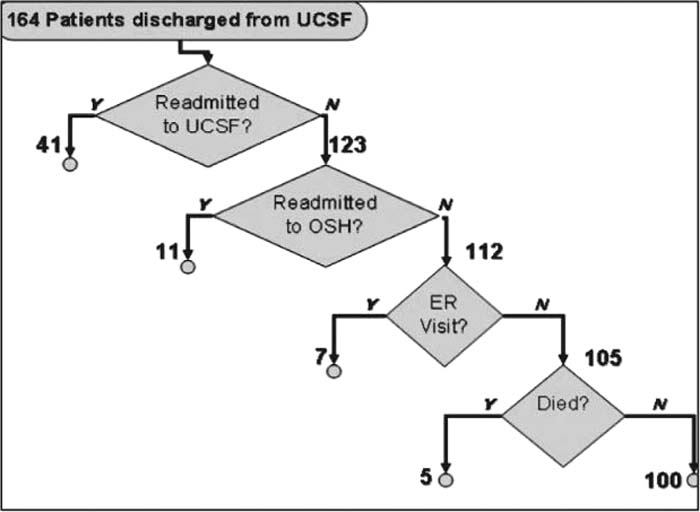
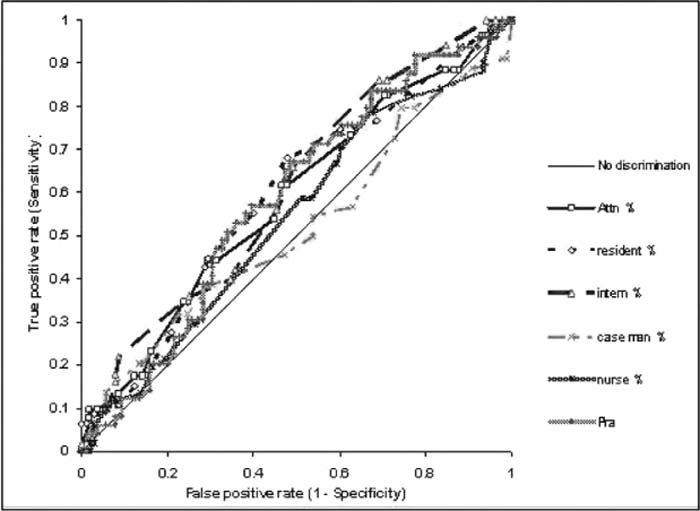
Patients ≥ 65 years old discharged from the general medical service at University of California, San Francisco Medical Center, a 550‐bed tertiary‐care academic medical center, were eligible for enrollment over a 5‐week period. At the time of discharge, the inpatient team members caring for each patient estimated the chance of unscheduled readmission to any acute care hospital within 30 days as well as the reason for potential readmission. Three methods were used to obtain a thorough capture of unscheduled readmissions: (1) EMR review at our own institution, (2) EMR review at the local county hospital, and (3) phone calls to patients/caregivers to determine readmission to an outside hospital. Discrimination was determined by creating ROC curves for each provider group and the Pra.
Results:
One hundred and sixty‐three patients were eligible for enrollment. Of these 163 patients, 5 patients died during the 30‐day period postdischarge. Of the remaining 159 patients, 52 patients (32.7%) were readmitted (Figure 1). Mean readmission predictions for the physician providers (attendings 32.3%, residents 29.4%, interns 31.2%) were closest to the actual readmission rate (32.7%), whereas case managers (38.7%), and nurses (43.6%) overestimated readmissions. The ability to discriminate between readmissions and nonreadmissions was poor for all provider groups and the Pra, as demonstrated by the ROC curves (Figure 2). None of the provider groups predicted reason for readmission with accuracy.
Conclusions:
As the first interdisciplinary readmission prediction study for general medicine patients, we found (1) larger than anticipated readmission rate when utilizing more thorough follow‐up and (2) poor ability of providers and an algorithm to predict readmissions. This study underscores the need for improved discharge planning and quality improvement in transitions in care for all elderly medicine patients.
Author Disclosure:
Nazima Allaudeen, none.