Case Presentation:
Genitourinary tract infections in adult men are typically bacterial in origin. However, fungal infections are a rare but serious cause of acute genitourinary pathology with notable morbidity. A 69‐year‐old African American man with diabetes mellitus (DM) presented with diabetic ketoacidosis. He endorsed dysuria without penile discharge or flank pain. Physical exam noted unilateral scrotal swelling with associated tenderness. Initial laboratory testing evidenced an elevated white blood cell count of 11.1 × 103/mL with pyuria, and urine cultures grew Candida albicans. Radiographic studies suggested epididymo‐orchitis with associated perineal abscess. Testing for HIV, N. gonorrhoeae, and C. trachomatis was negative. The patient developed C. albicans fungemia and required surgical debridement with orchiectomy in addition to flucona‐zole therapy. Pathology from surgical specimens supported C. albicans epididymo‐orchitis with associated inflammatory necrosis. After intensive treatment, the patient recovered without significant residual dysfunction.
Discussion:
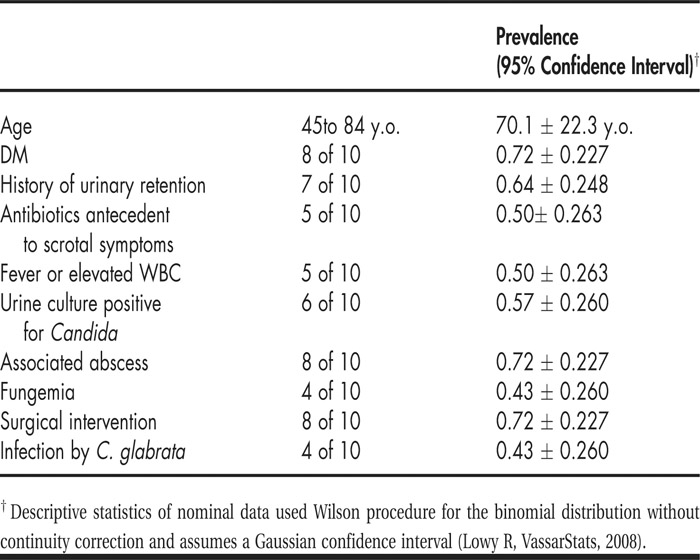
First documented in 1988, only 9 cases of Candida epididymitis/orchitis in adults have previously been reported in the English literature. Interestingly, these cases overwhelmingly occurred in patients with DM in the absence of comorbid immunocompromise, chronic indwelling urinary catheters, or systemic infection (see Table 1). The contribution of antecedent antibiotic treatments is unclear. Many Candida epididymo‐orchitis cases incurred significant complications and required surgical intervention in addition to antifungal therapy. The growing risk of nonalbicans Candida species in this disease influences appropriate antimicrobial selection. The scarcity of reported Candida epididymo‐orchitis despite the high incidence of Candida cystitis and funguria in hospitalized DM patients implies the disease may be underre‐cognized. Diabetics may be more susceptible to certain infections through multiple mechanisms, including impaired leukocyte function and enhanced Candida‐to‐epithelia adhesion; whether this susceptibility is a result of hyperglycemia or epiphenomena is uncertain. Further investigations into the pathophysiology of Candida genitourinary tract infections may provide insight into the optimal inpatient management of DM.
Conclusions:
Although rare, Candida epididymo‐orchitis carries considerable risk of complication. Clinicians should consider this disease when evaluating DM patients hospitalized with scrotal pain to prevent delayed diagnosis and prolonged inpatient care.
Disclosures:
P. C. Gandiga ‐ none