Background: Recent literature supports risk stratifying patients presenting to the Emergency Department (ED) with undifferentiated chest pain based upon the HEART score. Our institution utilizes the HEART score in a chest pain pathway. Patients with scores of 0 to 3 are typically discharged home after two negative troponins while those with intermediate scores of 4 and 5 are considered for further evaluation and hospitalization in our observation unit. The benefit of cardiac testing in the hospital for these patients is unclear. The objectives of this study were 1) to identify which factors might be predictive of diagnostic cardiac testing in patients hospitalized with HEART scores of 4 or 5 and to 2) to determine outcomes for these patients.
Methods: A retrospective chart review was performed to identify patients admitted to the UNC Observation Unit from the ED with a diagnosis of chest pain utilizing International Classification of Diseases, ver. 10 codes. We recorded demographics, HEART scores calculated by a hospitalist upon initial evaluation, whether Cardiology was consulted, and types of diagnostic testing performed. We also recorded 30-day outcomes for patients based upon ED revisits, return hospitalizations, clinic visits, myocardial infarction or Acute Coronary Syndrome, and mortality. We performed univariate and multivariate analyses to determine which demographic and clinical characteristics were predictive of diagnostic cardiac testing and 30-day outcomes.
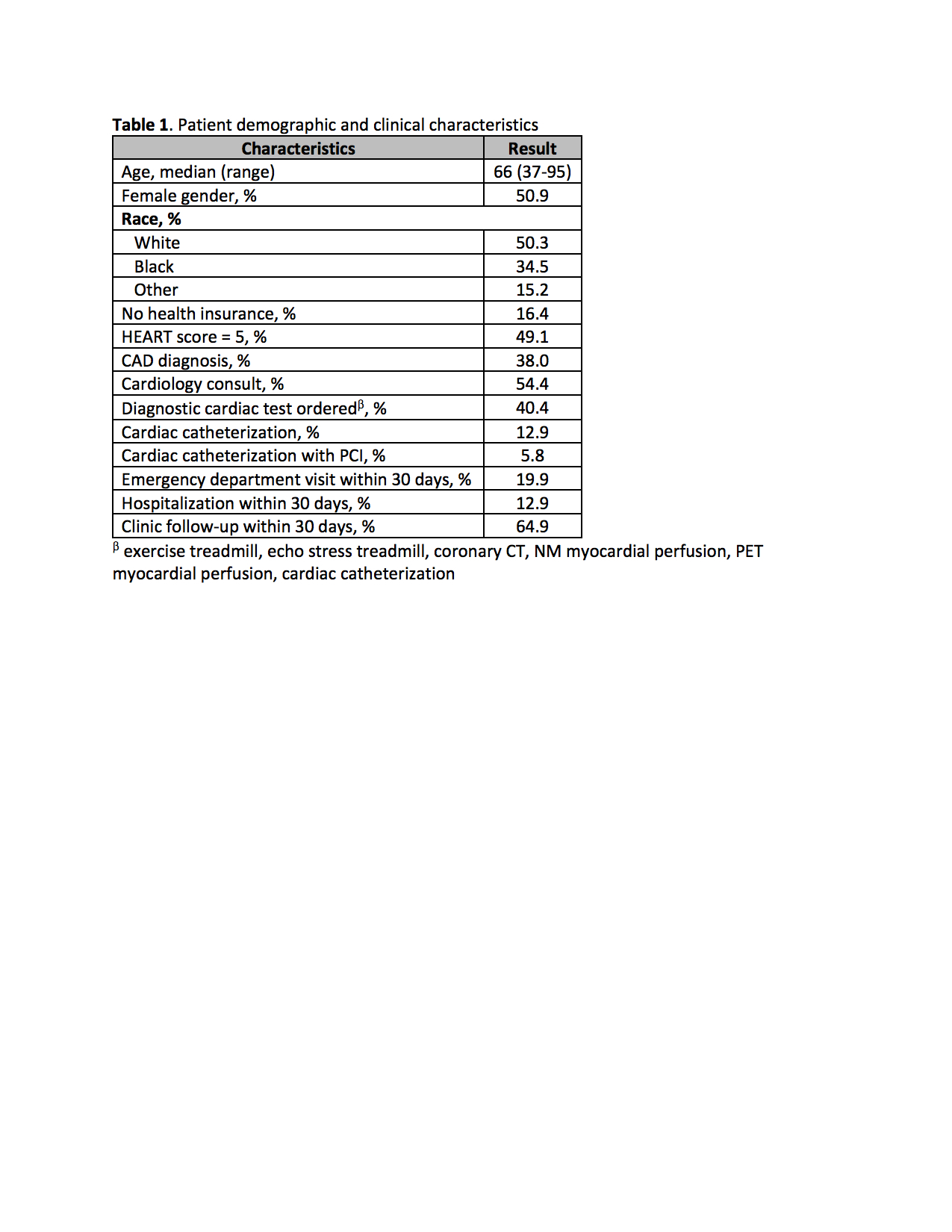
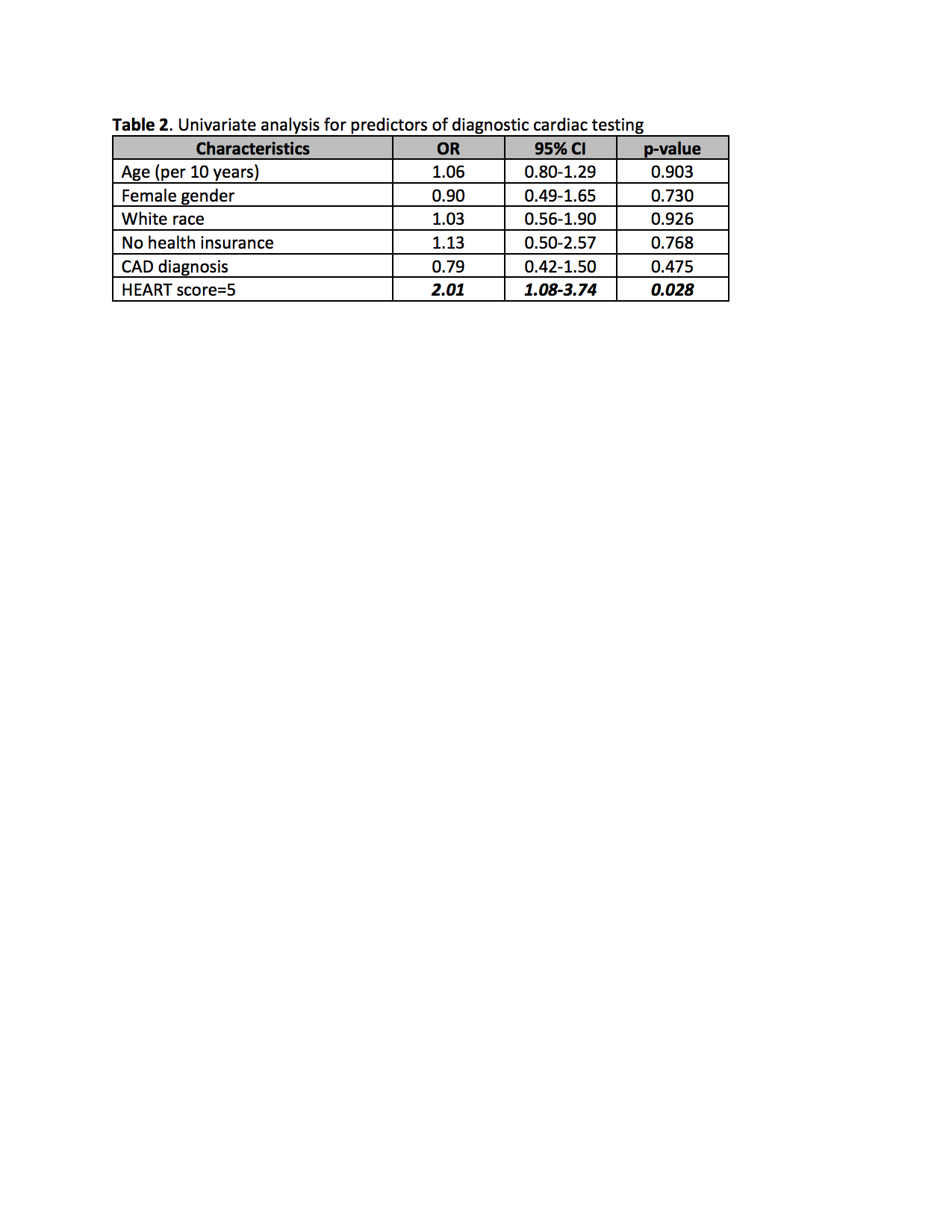
Results: We identified 171 patients hospitalized in our observation unit from the ED over a 6-month period with an initial presentation of chest pain and a HEART score of 4 or 5 (Table 1). Of these patients, 69 (40.4%) had cardiac testing during their hospitalization. A HEART score of 5 was predictive of further cardiac testing based upon both univariate analysis (Table 2) and multivariate analysis (OR 2.30, 95% CI 1.18-4.49). There were no factors predictive of 30-day outcomes.Among patients with HEART scores of 4 and 5, 22 (12.9%) underwent cardiac catheterization and 10 (5.8%) received a percutaneous coronary intervention (PCI). There were 7 patients with a HEART score of 4 who underwent cardiac catheterization and of those patients, three had a PCI. There were 15 patients with a HEART score of 5 who underwent cardiac catheterization and of those patients, 7 had a PCI. There were no patients identified as having an acute coronary syndrome or had died within 30 days of index hospitalization.
Conclusions: Cardiac testing was performed in 40% of patients identified as having a HEART score of 4 or 5. A HEART score of 5 was a predictor for further diagnostic cardiac testing likely due to higher risk for a major adverse cardiac event based upon prior studies and literature. However, only 5.8% of patients with a HEART score of 4 or 5 underwent cardiac catheterization and required a PCI. As no patients had an acute coronary syndrome or had died within 30 days of index hospitalization, this may be an area of further evaluation at our institution to potentially identify unnecessary cardiac testing in the hospital and improve resource utilization.