Background: Ventricular tachycardia (VT) is the most common cause of wide complex tachycardia and a potentially fatal cardiac rhythm disorder. Ventricular arrhythmias, including VT, cause approximately 25% of sudden cardiac deaths. Some studies have proposed a dose-response relationship between VT burden and risk of mortality; however, these studies may have been limited by the inclusion of a high number of false positive VTs. Our primary objective was to determine the association between VT burden and 30-day in-hospital mortality using a cohort of intensive care unit (ICU) patients with validated true VT events.
Methods: We conducted a retrospective observational cohort study of all adults admitted to the ICUs of a 600-bed academic medical center from September 2013-April 2015. ICU capacity comprised of 16 cardiac-ICU beds, 32 medical/surgical-ICU beds, and 29 neurological-ICU beds. Continuous cardiac telemetry data were used to develop a new algorithm at our institution to identify all potential VT events which were then expertly adjudicated and validated as true VTs. Patient-level data, including 30-day in-hospital mortality and electrocardiogram (ECG) abnormalities, were extracted from the electronic health record. Bivariable analyses were conducted using chi-squared tests and t-tests. Multivariable logistic regression modeling was conducted to determine whether VT burden was associated with 30-day in-hospital mortality.
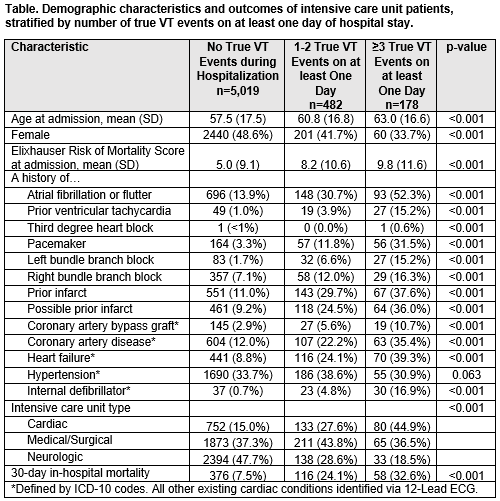
Results: Out of 5,679 consecutive hospitalizations, true VT events were identified in 660 hospitalizations (11.6%) over 64,553 total patient-days of follow-up. Among those who had at least one true VT event, the mean number of true VTs per day was 10.7 (standard deviation 59.2, range 1-1,206). Patients with VT were more likely to be hospitalized in the cardiac ICU and had more frequent underlying cardiac or ECG abnormalities (Table). Patients with 3 or more true VT events on at least 1 hospital day had a higher risk of in-hospital mortality (32.6%) compared to patients with 0 VT events (7.5%) and 1-2 VT events (24.2%) (p< 0.0001, Table). When compared to those who had 0 VT events, those who had 1-2 VT events on any hospital day were 2.5 times as likely to experience 30-day in-hospital mortality (OR 2.51, 95% CI 1.89-3.31), and those who had ≥3 VT events on any hospital day were 3.5 times as likely to experience 30-day in-hospital mortality (OR 3.52, 95% CI 2.29-5.40), after adjustment for baseline characteristics included in the Table.
Conclusions: Our study demonstrated that there are differences in patient characteristics when stratifying by number of VTs experienced on any day of hospitalization and increased VT burden is a significant predictor of 30-day in-hospital mortality. Quantifying VT burden using events per patient day could be a useful strategy to identify patients at high risk of 30-day in-hospital mortality.