Background: Prolonged immobility during hospitalization is associated with development of hospital-associated disability (HAD) and physical deconditioning. Physical therapy (PT) is important for HAD treatment and prevention but is a constrained resource in most hospital settings and planned sessions can be difficult to complete. Missing planned PT sessions, known as “PT non-treatment”, may compromise patient’s functional recovery and decrease therapist efficiency. However, little is known about the frequency or reasons for PT non-treatment and whether reasons for PT non-treatment are avoidable. We aimed to characterize PT non-treatment in patients hospitalized with acute medical illness.
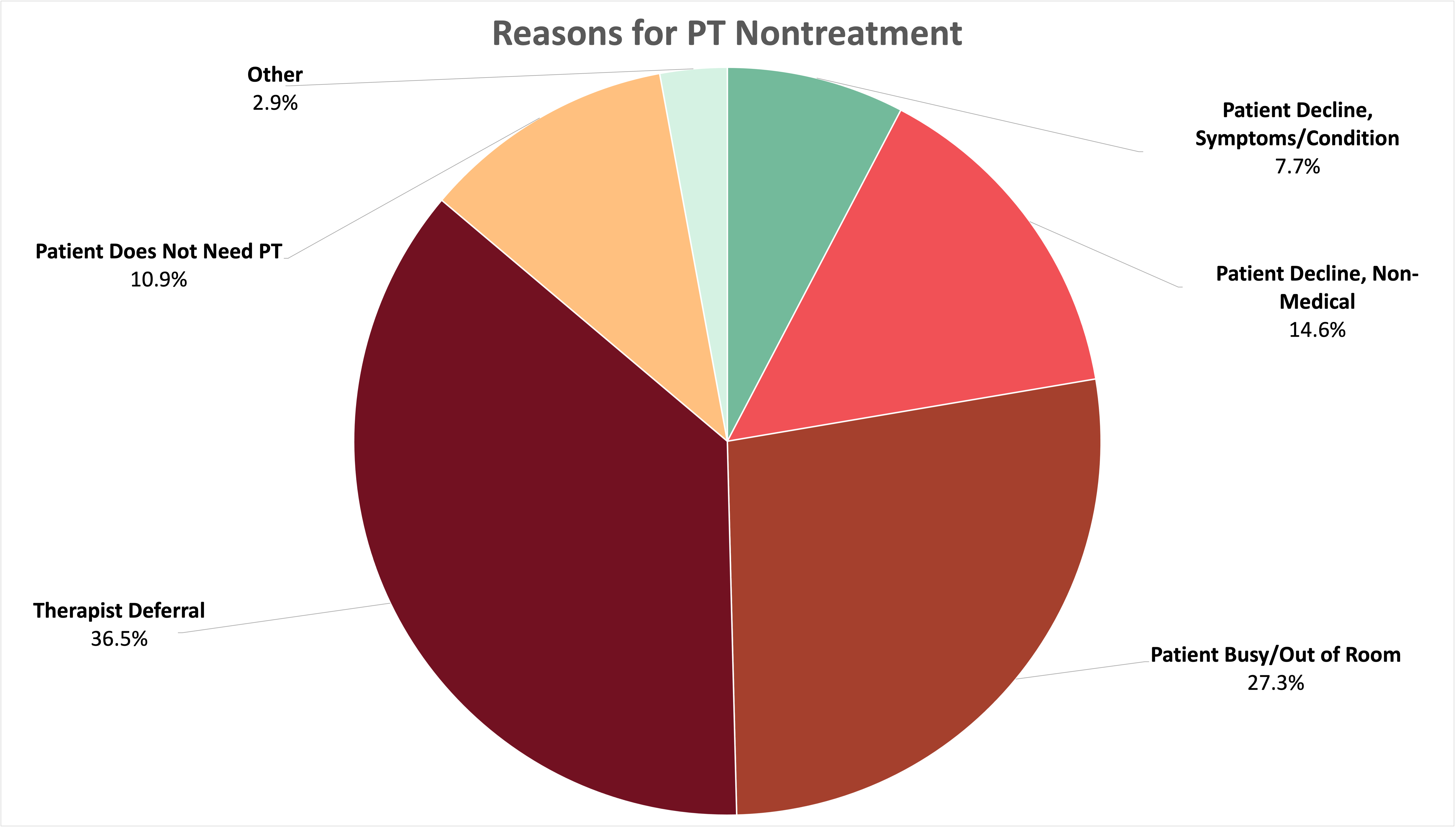
Methods: We conducted a retrospective analysis of patients admitted to the University of Chicago Hospital’s medical services between 8/2018 – 3/2021. We included patients > 50 years old with a length of stay (LOS) of 3-10 days and a mobility score indicating functional impairment at the time of admission [Activity Measure Post-Acute Care (AMPAC) score ≤ 18]. Descriptive statistics were used for to calculate patient characteristics and PT non-treatment rates and frequencies. A priori, we established the following categories for possible reasons for PT non-treatment: 1) patient declined due to symptoms/ condition, 2) patient declined for non-medical reasons, 3) patient unavailable due to imaging/treatment/busy with healthcare providers, 4) therapist deferred due to patient condition, 5) patient does not need PT, and 6) other. Poisson regression was used to test for associations between number of missed sessions and patient characteristics.
Results: We reviewed 3,364 admissions. Average age of patients was 73.0, 20.6% were female and 80.8% were Black. The average LOS was 5.9 days. Patients completed an average of 1.68 PT sessions per hospitalization and 24.4% of attempted PT sessions were missed without a same-day revisit for session completion. The most common reason for missed PT sessions was “therapist deferred due to patient condition” (36.5%) followed by “patient gone for imaging/treatment/busy with healthcare providers” (27.3%), “patient declined for non-medical reasons” (14.6%), “patient declined due to symptoms/ condition” (7.7%), and “other” (2.9%). Sessions were not completed due to the therapist deeming treatment unnecessary in 10.9% of cases. In adjusted analysis, factors associated with less PT non-treatment included age (β = -0.01; 95% Cl [-0.020,-0.003]) and higher functional mobility (β = -0.03; 95% Cl [-0.049,-0.004]). Longer LOS was associated with more PT non-treatment (β = 0.01; 95% Cl [-0.074,-0.156]). There was no statistically significant association between race or sex and PT non-treatment.
Conclusions: Our study demonstrates that nearly one-quarter of PT sessions scheduled for hospitalized patients are not completed. More than 60% of missed sessions are potentially avoidable with the implementation of quality or process improvement interventions. Educating patients on the importance of PT, coordinating patient scheduling, and improving ordering provider recognition of HAD and HAD risk factors could improve the patient-PT workflow optimizing the amount of time deconditioned patients spend with therapists.