Background: Penicillin class antibiotics are the most frequently reported drug allergy in the electronic health record (EHR), but recent studies find <5% of patients to be truly allergic. Nevertheless, EHR clinical decision support (CDS) software produces prolific drug-allergy alerts based on documented penicillin allergies that ultimately affect physician prescribing behavior. Inaccurately documented penicillin allergies in the EHR may promote inappropriate usage of alternate antibiotic classes for patients who otherwise could tolerate penicillin class antibiotics. We describe an approach using EHR audit trail data to characterize how drug-allergy alerts impact physician antibiotics orders for patients with documented penicillin allergies.
Methods: We analyzed EHR data containing inpatient medication orders and medication administration data from Stanford Health Care between 2008 and 2018. Chi-squared tests were used for significance. We first identified all orders for beta-lactam antibiotics (penicillin, cephalosporin, carbapenem, and monobactam class medications) amongst patients with documented penicillin allergies. We next cross-referenced drug-allergy alert data to discriminate between alerts that were ignored and alerts that resulted in cancellation of the order request. Medication administration record (MAR) records were used to confirm administration of ordered medications to the patient; these data further allowed identification of orders which administration was stopped for reasons including allergic reaction.
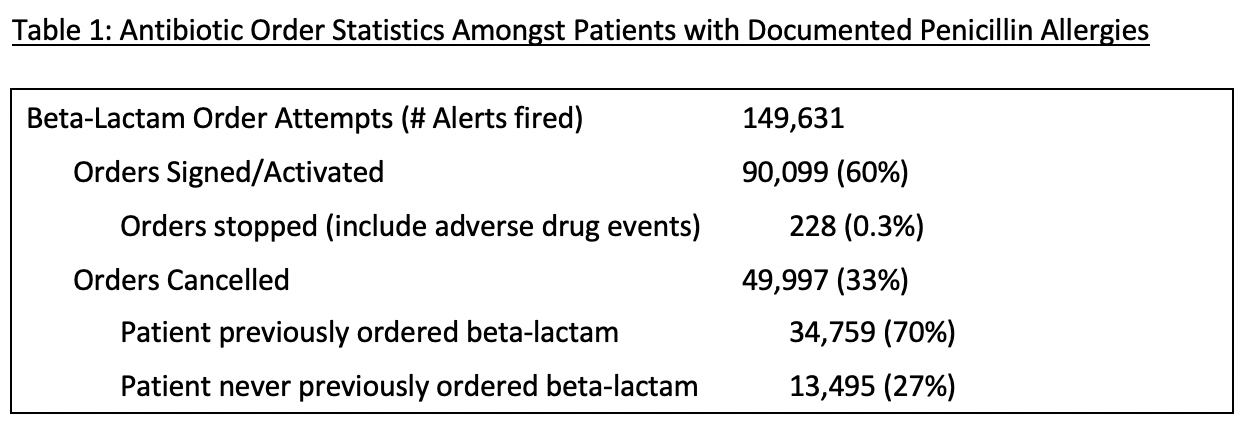
Results: Among the 133,795 patients with documented allergies to penicillins and/or cephalosporins, 33,389 (25%) received at least one inpatient order for beta-lactam antibiotics. Orders were signed and activated for 23,324 patients (17%); 206 (<1%) patients had administration stopped for some reason – including adverse drug reactions – while the remainder purportedly received and tolerated beta-lactam administration. Further, of the 19,085 penicillin-allergic patients for whom beta-lactam orders were at some point cancelled (reasons for cancellation include physician compliance with drug-allergy alert warnings), 11,595 (61%) patients had previously been ordered beta-lactams. See Table 1 for further summary statistics.
Conclusions: Our approach analyzing EHR audit trail data identifies instances in which CDS drug allergy alerts influence physicians to avoid prescribing their initially recommended penicillin-class antibiotics amongst patients that have previously demonstrated penicillin tolerance. Avoiding presumably first-line narrow spectrum penicillin-class antibiotics increases risk of antimicrobial resistance and directly opposes the goals of hospital antimicrobial stewardship; the opportunity for improvement is vast. Further analysis is needed to identify characteristics that may discriminate penicillin-allergic patients that receive beta-lactams from those who do not. This assessment informs an ongoing quality improvement initiative to improve antibiotic utilization amongst penicillin-allergics at our institution. We will soon be implementing a best-practice-alert (BPA) style CDS solution displaying historical penicillin-class antibiotic administration data within the medication ordering workflow. Indication of prior penicillin tolerance will help providers more accurately assess the truth and clinical significance of a documented penicillin allergy.