Background: Sickle cell disease (SCD) is characterized by lifelong, recurrent episodes of vaso-occlusive pain that often require inpatient hospitalization. Readiness for discharge is dictated by the patient’s pain intensity rated on the Numeric Rating Scale (0-10). Pain is an individualized multidimensional experience and a pain intensity score only measures one facet. Physical function is another component of acute pain that may be a better representation of a patient’s fitness for discharge. Unfortunately there is no well-established adult inpatient assessment tool. Using existing pediatric literature as well as scales from other diseases with chronic, unremitting pain we designed a new assessment. This scale is a functional status-based pain-assessment (FSPA) tool that was created with the hopes of improving evaluation of readiness for discharge.
Methods: The tool was created using input from a multidisciplinary team. FSPA helps assess the full spectrum of a patient’s functional limitations due to pain. FSPA consists of tasks that are recorded using the patient’s self-reported ability to complete a variety of activities ranging from easy to difficult. These activities included sleeping, walking around the room, etc. The patient’s perceived ability to complete tasks/activities were recorded using a 5 point Likert scale with choices ranging from “very easy” to “very difficult”. Concurrent numeric pain scores were also obtained. The tool was designed to be on a health literacy grade of one. The assessment was administered on a preselected nursing unit from January 2018 to June of 2019. Mean (standard deviation) or frequencies were used to summarize data. Pearson correlation was used to examine the relationship between the two continuous variables. We used exploratory factor analysis to determine factor loading and confirmatory factor analysis (CFA) using structural equation modeling for determining model fit and validation of the FSPA tool. We used item response theory analysis to determine the characteristics of each item using graded response model within a 2-parameter framework. All analyses were performed using Stata 14.0.
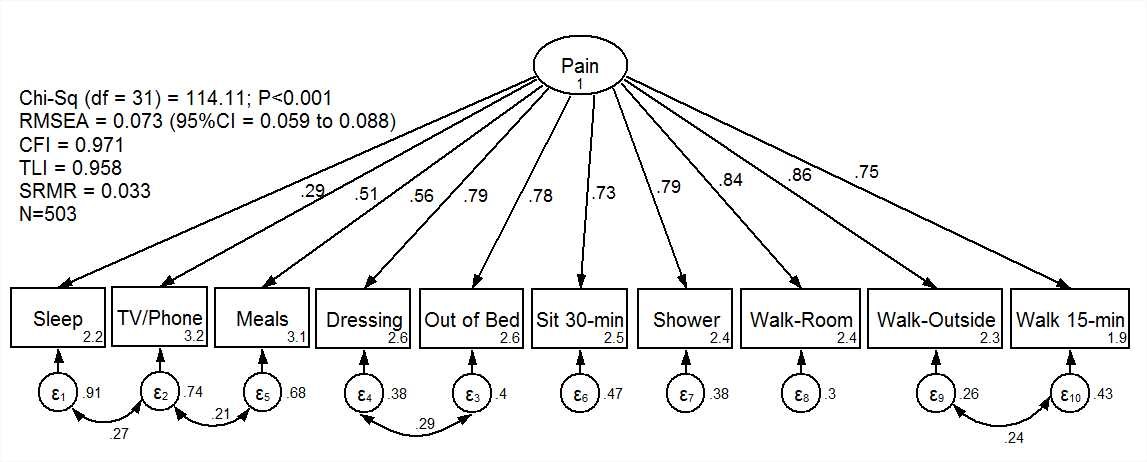
Results: During the study period, 504 assessments from 86 unique patients over 170 distinct admissions were completed. Of the 86 unique patients, 54% were females with mean age of 31.5 (SD8.0) years. The length of stay was 7.1 (SD6.9) days; minimum 0 days, max 38 days. Numeric Rating Scale mean was 6.8 (SD1.9) and of FSPA was 27 (SD8.0) the correlation between the two was -.4342 (p-value <.0001). In exploratory factor analysis, all questions from the questionnaire loaded on a single factor highlighting strong construct and face validity. The CFA found adequate convergent and discriminant validity and showed strong fit of the model to the data using routine diagnostic statistics (Figure). Using item response theory analysis, we found that the item discrimination varied from 0.56 to 4.1 while difficulty of the items covered broadly the latent variable of the functional status with pain with values ranging from -2.8 to 7.5.
Conclusions: We have developed and validated a functional assessment for adult inpatients. This assessment may improve the evaluation of readiness for discharge in adults with sickle cell disease by trending the evolution of pain’s impact on the patient’s day to day abilities. Future research will need to be performed to evaluate if FSPA compares to other previously established functional assessment tools as it could have an enormous impact on hospital length of stay.