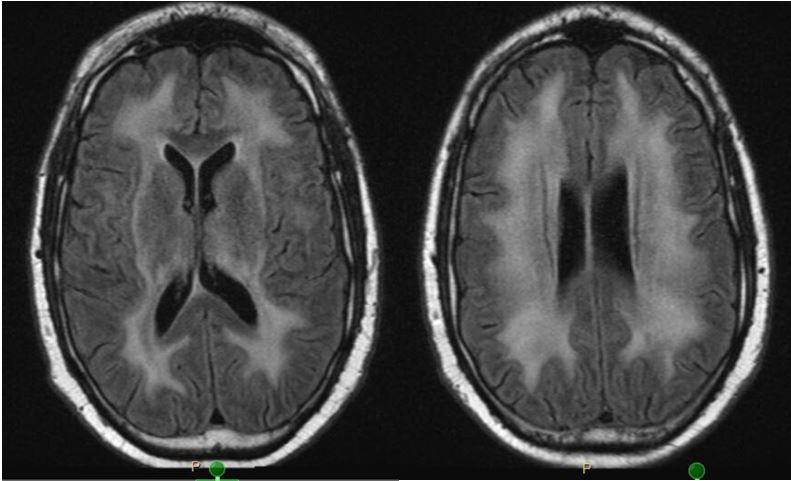
Case Presentation: A 33 year old male with systemic lupus erythematosus (SLE) complicated by recurrent diffuse alveolar hemorrhage (DAH) presented with ataxia, lethargy, cough, and dyspnea. He had been recently exposed to high intensity immunosuppression for his DAH as it was thought to be secondary to SLE. However, it was later diagnosed as herpes simplex virus (HSV) and pneumocystis jiroveci pneumonia. Given his neurological symptoms and immunosuppression, a brain MRI was obtained and revealed ubiquitous white matter enhancement. He did not have focal sensory or motor deficits. He had no history of traumatic or hypoxic brain injury. He had not been on any medications known to cause leukoencephalopathy. Lumbar puncture showed a significantly elevated protein level at 270 mg/dL, no leukocytes, negative ribosomal protein P, no oligoclonal bands, and two negative JC virus PCR tests. Serum HIV antigen, antibody, and RNA PCR testing was all negative. Very long chain fatty acid profile was negative, ruling down leukoadrenodystrophy. While declining illicit drug use initially, the patient later admitted to smoking heroin and uncovered the diagnosis of heroin inhalation toxic leukoencephalopathy (HIL).
Discussion: Leukoencephalopathy describes pathologic, diffuse white matter changes with associated neurological issues. Toxic leukoencephalopathy is a specific subset of leukoencephalopathy related to exposures to substances including heroin, methamphetamine, carbon monoxide, or even medications like methotrexate. Hypoxic injury and severe hypertension may also produce a similarly appearing brain MRI. HIL is characterized by ataxia, apathy, signs of upper motor neuron injury, hyperpyrexia, and eventually death in as high as 48% of patients. Diagnosis is based on characteristic imaging, a history consistent with inhaled heroin use, and the absence of another more likely cause. Treatment is supportive and also involves avoiding continued exposures (Tormoehlen, 2013).
With knowledge of this entity and adequate history, extensive and sometimes dangerous workup, like lumbar puncture, may be avoided. Also, discovery of issues including substance abuse and carbon monoxide exposure may lead to lifesaving interventions.
Conclusions: HIL is a rare form of toxic leukoencephalopathy related to inhalation of heroin. It presents with vague symptoms such as apathy and ataxia but may be fatal in a large portion of patients. Knowledge of this entity and asking appropriate social history questions can lead to prompt diagnosis and decrease unnecessary testing. Early diagnosis may also allow for adequate substance abuse resources to be provided and protect others from dangerous exposures such as carbon monoxide poisoning.
Reference:
1. Tormoehlen LM. Toxic leukoencephalopathies. Psychiatr Clin North Am. 2013;36(2):277-92