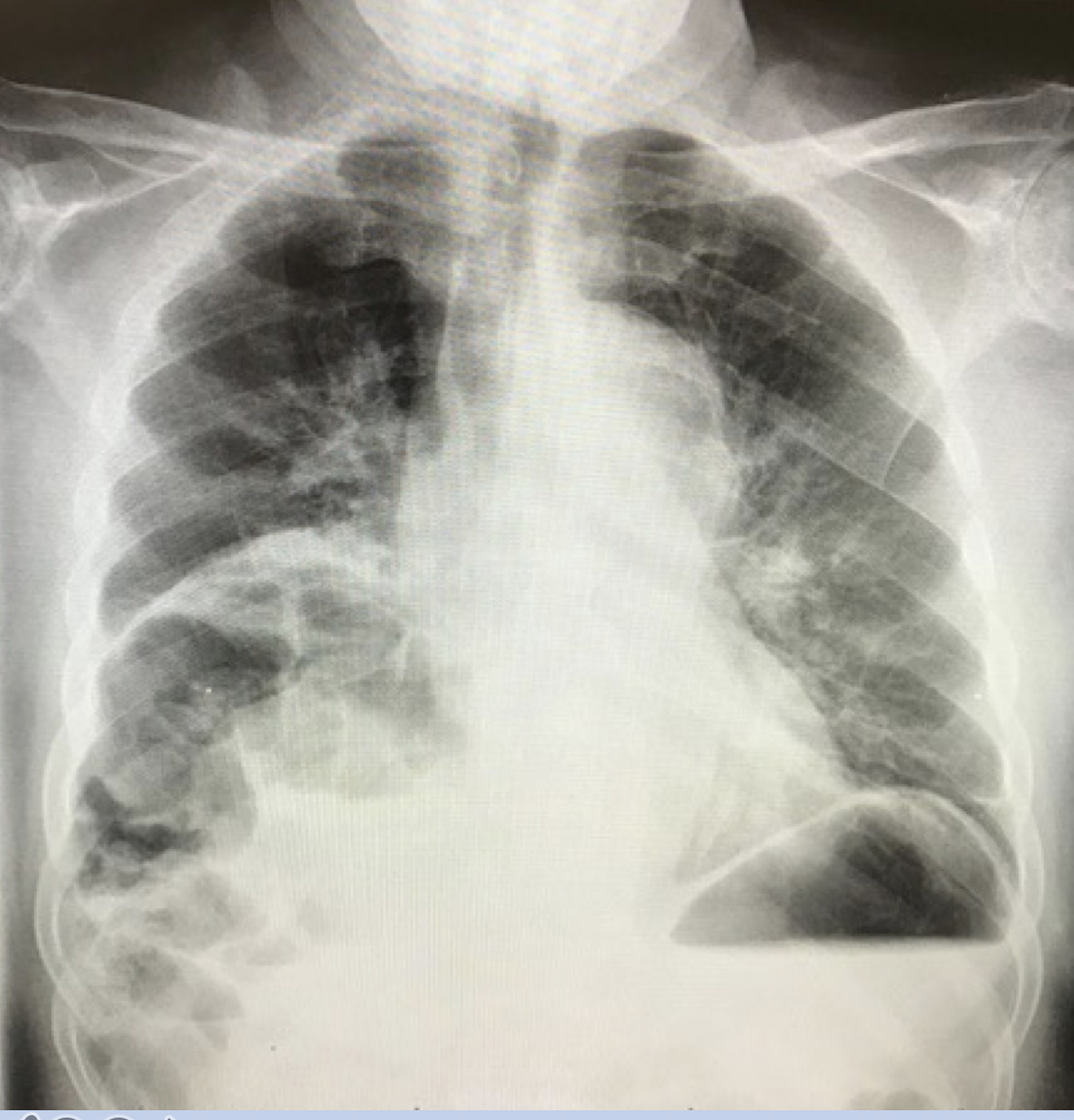
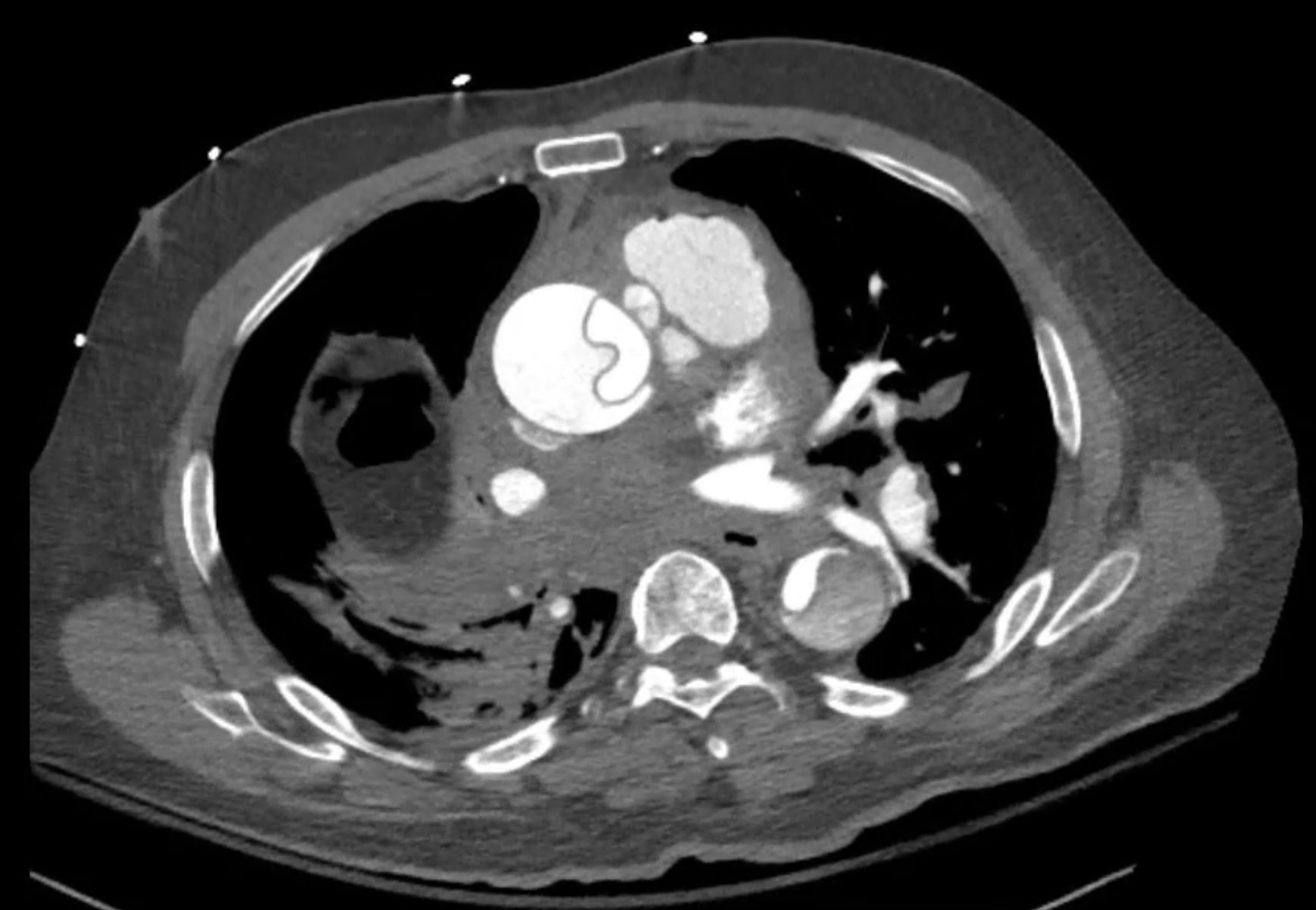
Case Presentation: A 71-year-old-male with history of HTN, tobacco abuse, and Hepatitis C cirrhosis complicated by hepatocellular carcinoma (HCC), was admitted following transarterial chemoembolization (TACE) for HCC. TACE of a 3.2cm left hepatic lobe mass was performed. Access was obtained via the right common femoral artery. No immediate complications were noted, and the patient was transferred to hospital medicine for monitoring. He subsequently complained of severe, anterior chest pain and dyspnea. He was afebrile, with a HR 106, RR 24, BP 79/51 (right arm), 82/57 (left arm), and oxygen saturation of 94% 2L/min nasal cannula, and was in acute distress. Physical exam was notable for tachycardia (with a regular rhythm), tachypnea, diffuse expiratory wheezing and dry rales, and right upper quadrant abdominal tenderness, with an otherwise unremarkable abdominal exam. His right lower extremity was cold and dorsalis pedis and posterior tibial pulses were not palpable. Labs revealed a WBC 16,600 u/L with neutrophil 75%; hemoglobin and platelets were within normal limits. His renal panel and liver function tests were baseline. Troponin was elevated to 0.25 ng/mL, BNP 301 pg/mL, high sensitivity d-dimer 66,400 ng/mL, and lactic acid 5.1 mmol/L. EKG showed sinus tachycardia and frequent PVCs, but no acute ST-segment or T-wave changes. CXR was notable for multifocal patchy parenchymal opacities. CT pulmonary embolism protocol could not be obtained emergently due to contrast allergy (angioedema). STAT transthoracic echocardiogram was obtained which demonstrated a Stanford Type A aortic dissection. Fluids and other supportive care were delivered and the patient was rapidly pre-medicated with steroids. CT angiogram demonstrated a Type A dissection, extending from the aortic root to the right external iliac artery, hemopericardium, extrinsic compression of the right pulmonary artery, obstruction of the left renal artery, and obliteration of the right external iliac artery. He was taken to the operating room emergently for extensive interdisciplinary surgical management.
Discussion: Type A dissection is not a previously described complication of TACE. The most common complication is post-TACE syndrome which is a constellation of fevers, vomiting, and severe abdominal pain. Others may include vascular access site injuries (hematoma or pseudoaneurysm), hepatic artery injuries, off-target embolization, pulmonary embolism, or acute liver injury. This patient did have vascular risk factors including HTN, smoking history, and vascular calcifications seen on imaging, thereby increasing risk for iatrogenic dissection.
Conclusions: TACE is a generally safe treatment option for HCC in patients who meet indications for the procedure. Arterial access is usually accomplished using a catheter much smaller in size than that used in other arterial procedures, such as left heart catheterization, which thereby mitigates some of the vascular injury risk associated with these procedures. Despite this, complaints of chest pain and vital sign instability after vascular access should trigger a broad differential including acute dissection regardless of the catheter size, and physicians should be familiar with various imaging modalities that may be utilized to diagnose aortic dissection.