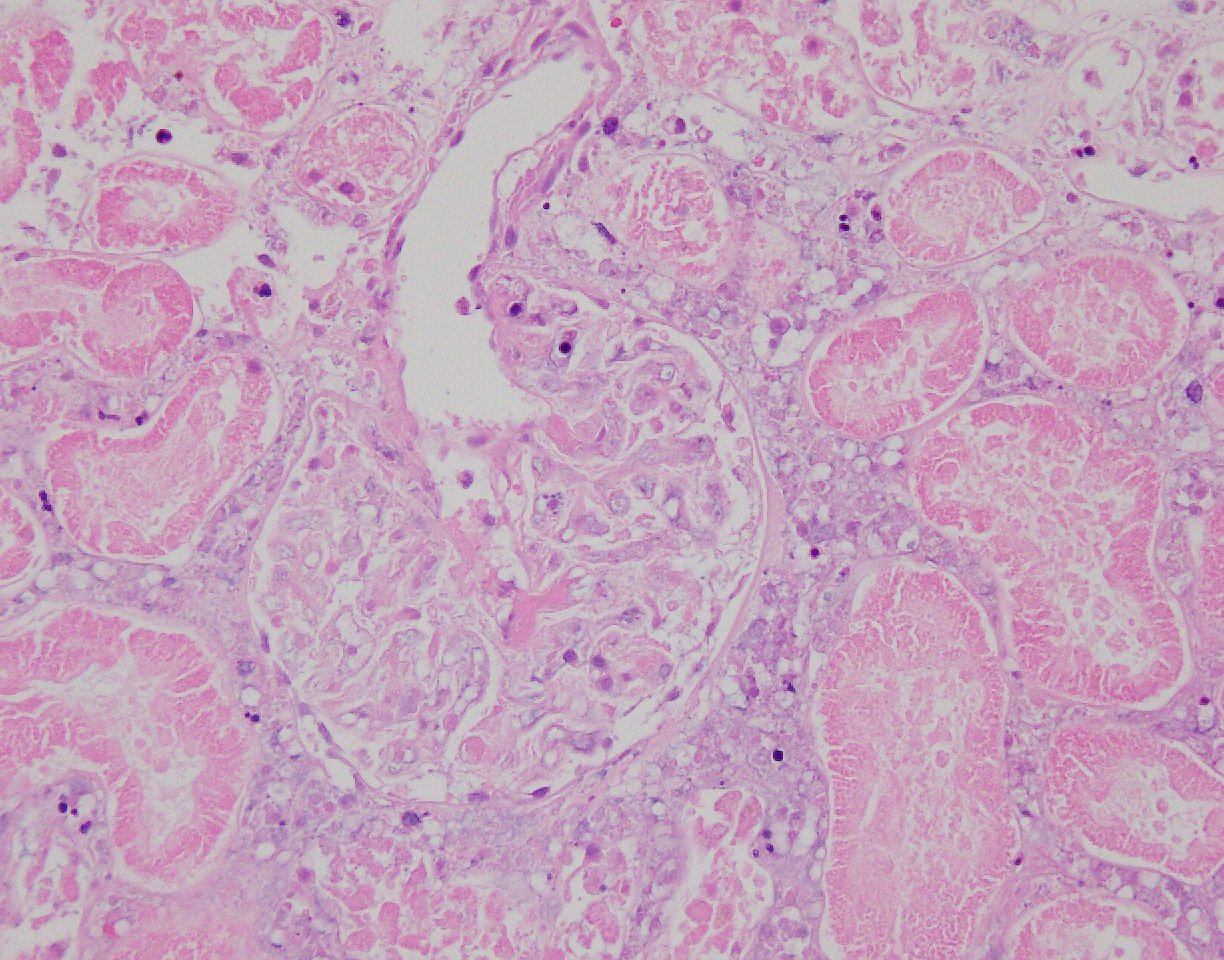
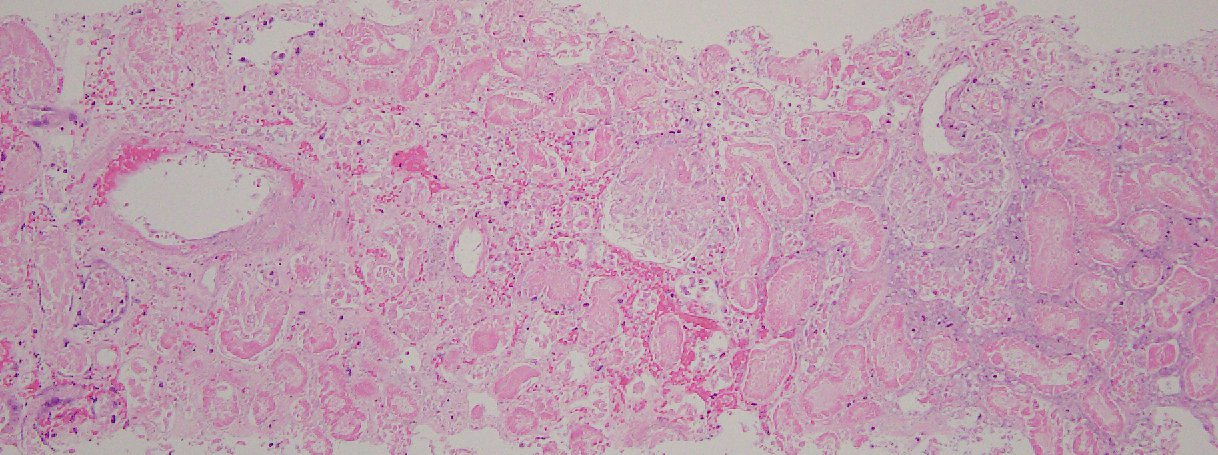
Case Presentation: A 102-year-old male with a past medical history of coronary artery disease(CAD), transient ischemic attack(TIA) ,well controlled hypertension(HTN), presented to emergency department(ED) with aphaisa and left facial droop of two hours duration. His symptoms were resolved by the time he presented to the ED. Surgical, social, and family histories were unremarkable.Physical Examination was benign . Complete blood count, metabolic panel, lactic acid, troponin and urine analysis were within normal limits. No concerning findings were noted on head CT or EKG. Echocardiogram showed preserved ejection fraction with no patent foramen ovale or thrombus. MRI of the head was negative for any acute disease. The patient was admitted to the stroke floor and initiated on aspirin, and a statin for a suspected TIA. Subsequently over the next two days, he developed left flank pain, elevation of blood pressure along with a rise in creatinine >0.5mg/dl from baseline. Urinalysis showed microscopic hematuria and mild proteinuria, and Nephrology was then consulted. Non contrast CT of the abdomen/pelvis was done which ruled did not reveal any acute medical or surgical pathology. Subsequent work up revealed low C3 but other autoimmune, vasculitis and hepatitis panels were negative . Coagulation panel was benign. Renal Artery duplex did not reveal any hemodynamically significant stenosis. Due to worsening of renal function and worsening oligo-anuria, the patient was initiated on hemodialysis. He sunsequently underwent a renal biopsy for a definitive diagnosis. Pathology showed 90% subacute ischemic cortical renal artery infarction, likely from athero-embolic etiology. Over the remainder of the hospitalization, his blood pressures stabilized and his urine output improved . He was discharged with outpatient hemodialysis and strict management of his athero-embolic risk factors. And upon follow- up, at approximately two months after discharge, he regained enough renal function to be able to come off dialysis. He currently has CKD Stage V, but is stable and doing well.
Discussion: Atheroembolic Renal Disease(AERD) results in occlusion of small arteries/arterioloes by cholesterol crystals from ulcerated/ruptured aortic atherosclerotic plaques either a) spontaneously or b) Iatrogenic – by dislodgement of athero-emboli after invasive cardiovascular procedures. The skin, gastro intenstinal tract, kidneys and brain, are the common organs involved. Renal biopsy may be required to for a definitive diagnosis in cases of renal involvement. Treatment is mostly supportive and includes, antiplatelets ,statins. Our case highlights the evaluation of AERD in a patient with risk factors for atheroembolism (age >50,HTN,DM, history of TIA, CAD, tobacco use, invasive cardiovascular procedure) who presented with new onset abdominal pain, accelerated HTN, AKI, mild proteinuria, hypocomplementemia and hematuria. He was presumed to have AERD based on his renal biopsy, which showed extensive renal infarction. Prompt antiplatelet and statin therapies, HTN optimization, dialysis initiation played an essential role in his renal recovery
Conclusions: AERD needs a high index of suspicion for prompt diagnosis and management as it is associated with a high mortality. Treatment is supportive and management of athero-embolic risk factors is crucial. Risk of recurrent embolic insults is high. Chronic Kidney disease, ESRD and multi organ failure are the most common complications.