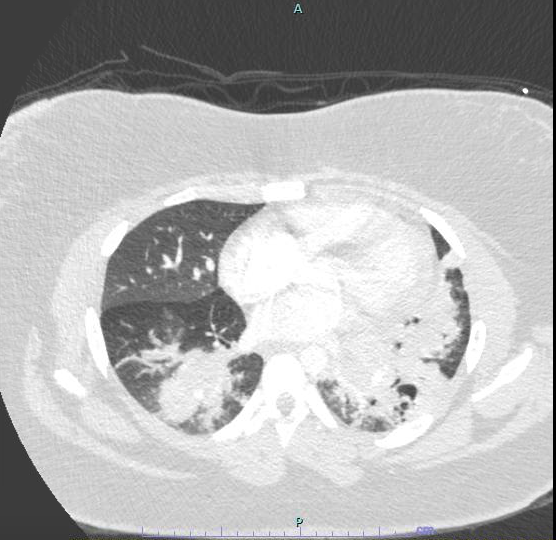
Case Presentation: 17 year old female with history of severe persistent asthma, allergies, and chronic marijuana use presents with one month of worsening dyspnea, cough, and chest pain, after treatment for left lower lobe pneumonia and asthma exacerbation.She was afebrile, tachycardic, tachypneic, but saturating well on room air. Lung exam had diminished breath sounds at left base and mild expiratory wheezing. Chest x-ray showed worsening bilateral lower lobe airspace disease, and ultrasound showed very small left pleural effusion. CT pulmonary angiogram ruled out pulmonary embolism and showed extensive bilateral airspace disease with multiple areas of cavitation in left lower lobe concerning for necrotizing pneumonia.She was initially started on antibiotics, but found to have negative TSPOT, HIV, Pneumocystis, beta D-glucan, procalcitonin, urinary Legionella and Strep Pneumoniae antigens, and negative CD4/CD8 flow cytometry. Immunologic studies showed negative ACE, cANCA, pANCA, anti-DNA antibody, C3, C4, anti-PR3, myeloperoxidase, and normal immunoglobulin panel. Bronchoalveolar lavage showed fibrinous tissue casts with eosinophils, as well as peripheral eosinophilia. Empiric treatment with pulse IV steroids was initiated with improvement in respiratory symptoms. She underwent diagnostic video-assisted thoracoscopic lung biopsy, confirming chronic eosinophilic pneumonia (CEP).Hospital course was complicated by supraventricular tachycardia from hemopneumothorax that required replacement of chest tube and poor wound healing due to chronic steroid therapy. She was discharged home with oral steroid therapy and subsequently started on mepolizumab.
Discussion: Idiopathic CEP is rare, typically less than 3% of interstitial lung disease, which affects women more than men, in all age groups with mean age around 45 years at diagnosis. Patients typically have a history of asthma or atopy, and symptoms of dyspnea, cough, fever, weight loss and rarely chest pain and hemoptysis.Our patient’s hospital course was prolonged by delays in diagnostic testing because CEP secondary to marijuana is not well characterized. In fact, acute eosinophilic pneumonia (AEP) typically causes respiratory failure in the setting of marijuana and other drug or inhalant use. Though more dramatic in presentation, AEP treatment is short term while CEP demands chronic duration of steroids or biologics, each carrying both clinical and economic burden. For our patient, persistent complications secondary to chronic steroid use led to recurrent hospitalizations. While biologics, currently approved for the treatment of severe eosinophilic asthma, show promise to wean systemic steroids, they too come with financial cost.
Conclusions: Chronic eosinophilic pneumonia is increasingly becoming recognized as a complication of marijuana smoking, particularly with history of atopy or asthma that is poorly controlled despite medication adherence. Symptoms and treatment of CEP are costly and frequently recurrent. Given the increasing availability of marijuana to adults and youth, clinical complications secondary to marijuana use, such as CEP, must be considered.