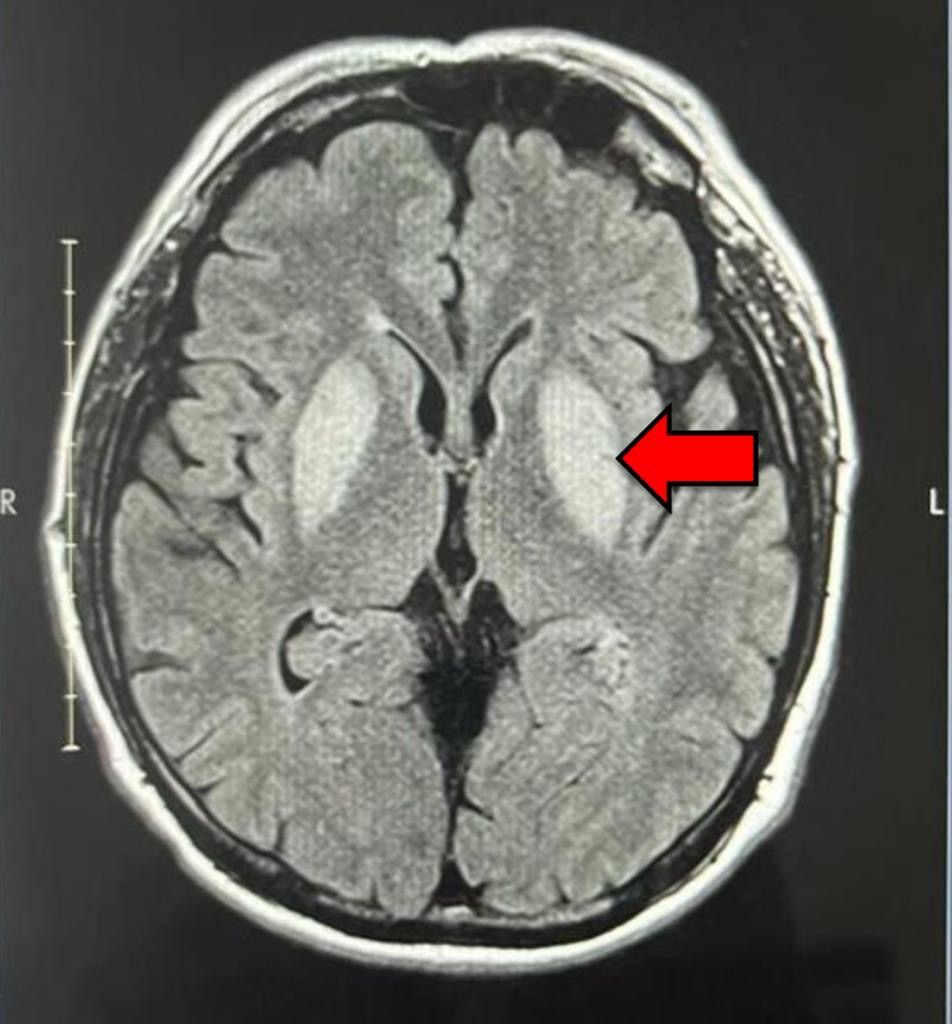
Case Presentation: A 57-year-old Hispanic male presented with an episode of syncope while at his workplace. He is a Pest Control Technician and had a 7-year history of exposure to organophosphates. He had a history of frequent falls over past six months and had no exposure to other toxic substances, alcohol or drugs. Physical exam was consistent with resting tremor, slurring speech and ataxic gait [4,5]. Further workup with CT head revealed internal capsule enlargement and edema within bilateral basal ganglia without signs of hemorrhagic transformation [2]. Subsequent MRI Brain indicated edema and abnormal signal involving bilateral basal ganglia, extending to the cerebral peduncle [2]. Additionally, a finding of restricted diffusion was noted within the medial aspect of the Globus pallidus suggestive of necrosis [2]. Cerebrospinal fluid (CSF) analysis was performed to rule out infectious, autoimmune, and paraneoplastic etiologies, and the results were unremarkable. After discussion with Neurology and Radiology, it was determined that patient’s presentation was consistent with bilateral basal ganglia involvement due to chronic organophosphate exposure. Over the course of admission, he showed continued clinical improvement and was eventually discharged and advised to avoid organophosphate indefinitely [1].
Discussion: Organophosphate exposure has been associated with various neurological effects including tremors, ataxia, slurring of speech and basal ganglia involvement like Parkinson’s disease [1,3,4]. Acute organophosphate toxicity is well documented and is characterized by an initial acute muscarinic syndrome, followed by a nicotinic phase. In contrast, chronic exposure often eludes timely diagnosis and appropriate management as no cholinergic symptoms are seen [2]. During hospital stay, patients clinical improvement could be solely attributed to symptomatic and supportive treatment, more importantly cessation of exposure to organophosphates. In conclusion, this case underscores the intricate interplay between occupational exposure, neurological manifestations, and radiological findings.
Conclusions: This case report emphasizes the significance of occupational history taking, considering toxic exposures, collaborating with other specialties and promoting health and prevention. Recognizing that the improvement of symptoms can occur with the avoidance of further exposures serves as a valuable learning point [1].