Background: Thromboprophylaxis of hospitalized COVID-19 patients – including extended, post-discharge thromboprophylaxis in high-risk patients – has been evaluated in multiple randomized trials and incorporated into antithrombotic guidelines. Yet, provider adoption of best practices remains sub-optimal. Our aim was to assess whether an electronic health record (EHR)-agnostic clinical decision support (CDS) tool incorporating the validated IMPROVE-DD venous thromboembolism (VTE) risk score, embedded within clinical workflows, increases appropriate thromboprophylaxis and improves clinical outcomes in this population.
Methods: This was a subgroup analysis of a multicenter cluster randomized trial (NCT04768036) of a platform-agnostic CDS tool integrated with thromboprophylaxis order entry. Patients over 60 years of age admitted for COVID-19 with additional risk factors as per the IMPROVE-DD VTE risk score were included. The primary outcome was the rate of appropriate thromboprophylaxis among at-risk and high-risk patients per IMPROVE-DD VTE score thresholds, both at hospital admission and discharge. Key secondary outcomes included rates of VTE, arterial thromboembolism (ATE), total thromboembolism (TE), major bleeding, and all-cause and VTE-related readmissions at 30 days post-discharge.
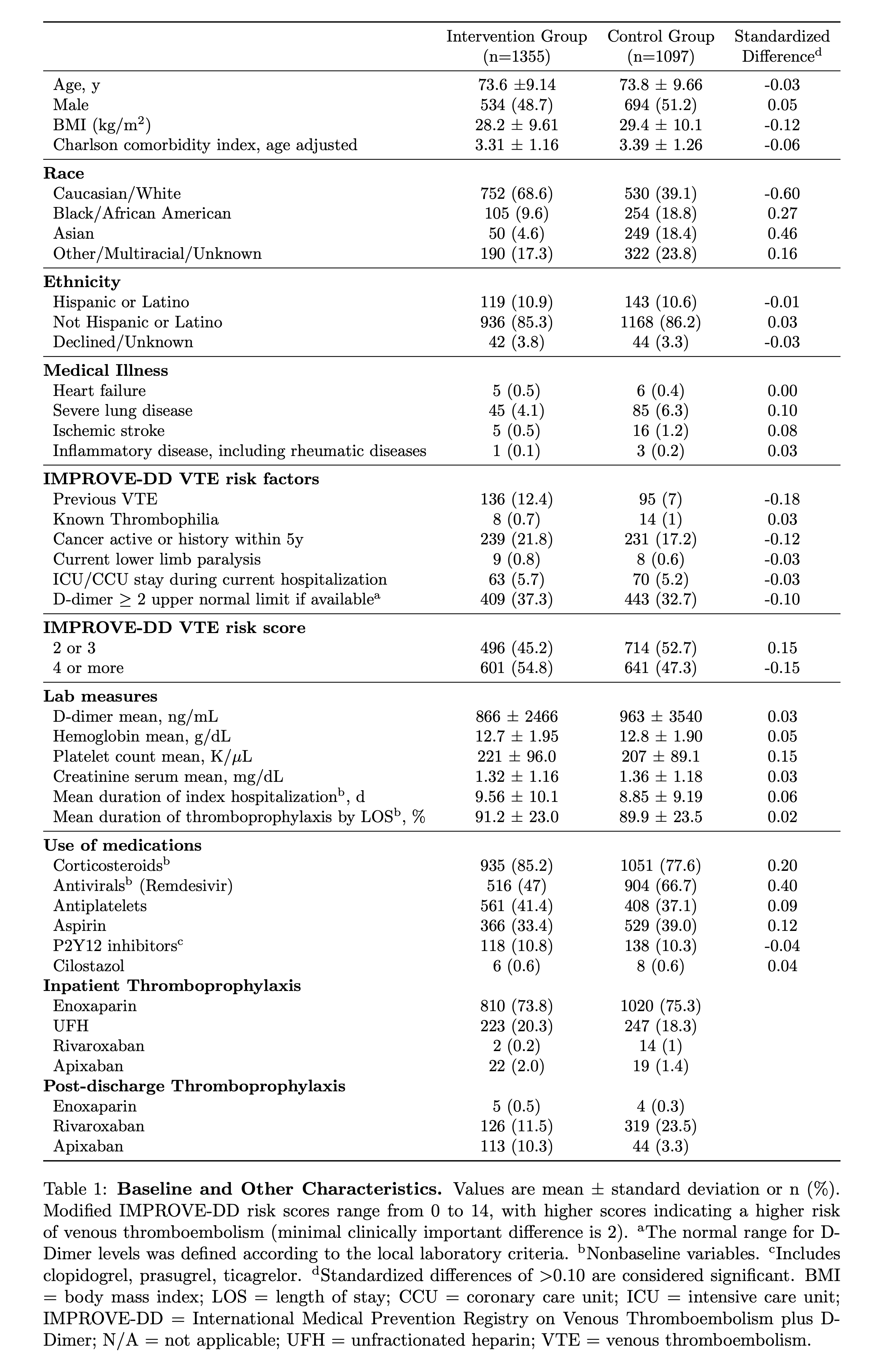
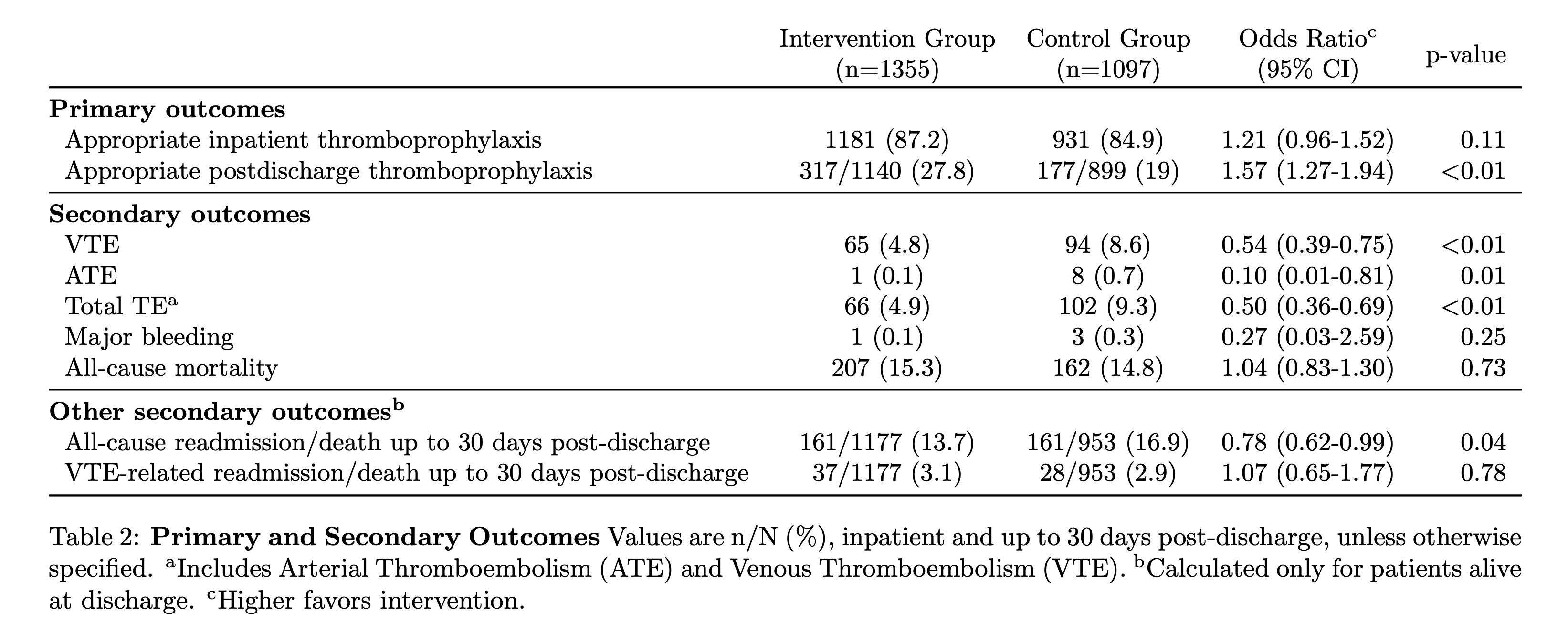
Results: From December 21, 2021, to January 21, 2022, 2,452 hospitalized COVID-19 patients were randomized to two clusters of two tertiary hospitals each (1097 patients in the usual care group and 1355 patients in the intervention group using the CDS). Baseline and other characteristics are shown in Table 1. For the primary outcome, there was a numerical, but non-statistically significant, increase in appropriate inpatient thromboprophylaxis (87.2% versus 84.9%), and a significant increase in at-discharge extended thromboprophylaxis in high-risk COVID-19 patients in the intervention group (Odds Ratio (OR) 1.57, 95% Confidence Interval (CI) 1.27-1.94, p< 0.001) (Table 2). For secondary outcomes, there were significant reductions in VTE (OR 0.54, 95% CI 0.39-0.75, p < 0.001), ATE (OR 0.10, 95% CI 0.01-0.81, p=0.01), and total TE (OR 0.50, 95% CI 0.36-0.69, p < 0.001) in the intervention group (Table 2). There were no differences in major bleeding, all-cause mortality, and VTE-related readmission/death between groups, while there was a marginally significant reduction in all-cause readmission/death in the intervention group (OR 0.78, 95% CI 0.62-0.99, p=0.04).
Conclusions: An EHR-agnostic CDS tool incorporating the IMPROVE-DD VTE score increased appropriate at-discharge extended thromboprophylaxis in high-risk hospitalized COVID-19 patients. This change in provider behavior was associated with reduced major thromboembolism including VTE, ATE, and total TE without increased major bleeding. The composite of all-cause readmission or death was also reduced in the intervention group. Our CDS tool holds promise in reducing major thromboembolic outcomes among hospitalized COVID-19 patients, especially as it is designed to be interoperable with any EHR platform.